Obstructive sleep apnea (OSA) is a common sleep disorder that impacts up to 30% of the U.S. population. Individuals with OSA repeatedly experience brief episodes in which their breathing is restricted or paused during sleep due to obstructions in the airway.
Without treatment, OSA can lead to a variety of health consequences, including daytime tiredness and an increased risk of other health conditions. Fortunately, several treatment options for OSA are available, including positive airway pressure (PAP) devices, oral appliances, and surgery.
Although PAP devices that deliver continuous positive airway pressure (CPAP) therapy are the preferred treatment for many people with OSA, newer treatment options are emerging. Learn about nasal expiratory positive airway pressure (EPAP), an alternative to CPAP that may benefit some people with OSA.
What is Expiratory Positive Airway Pressure (EPAP)?
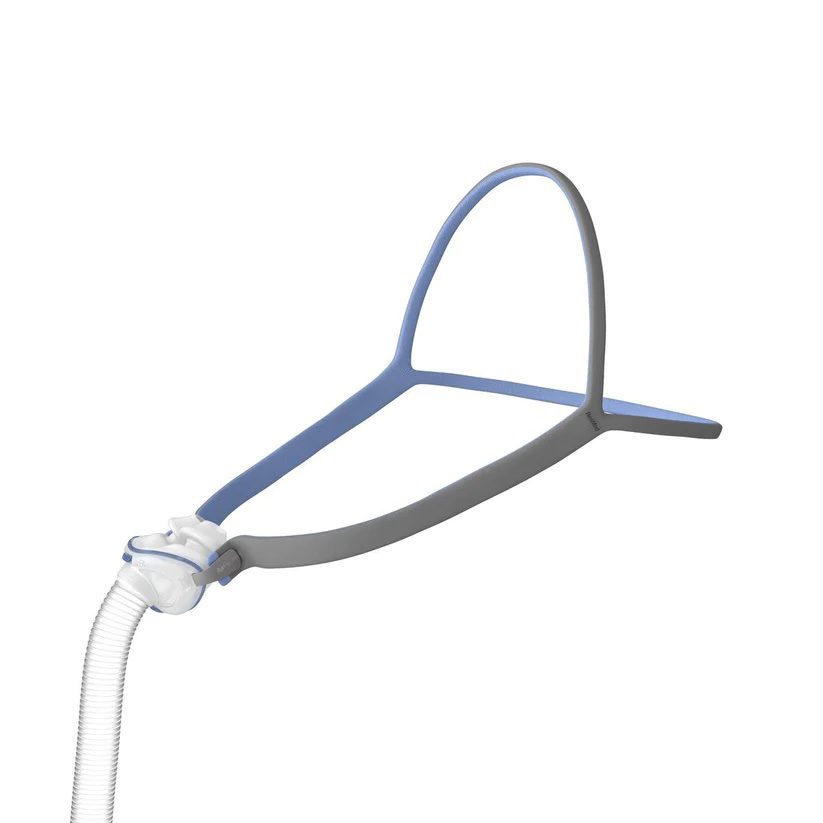
Nasal expiratory positive airway pressure (EPAP) is an emerging therapy for obstructive sleep apnea. An EPAP device consists of two valves that cover the nostrils as a person sleeps. When the sleeper exhales, these valves limit airflow and create sufficient pressure within the airway to prevent it from collapsing.
Unlike other PAP therapies, nasal EPAP doesn’t require a mask to keep the airway open during sleep. Instead, valves are secured in the nostrils or held in place with a strap that fits securely around the back of the head.
Although additional research is needed, several studies suggest that EPAP may be effective at improving symptoms for some people with OSA.
In one study, about half of the study participants had a 50% reduction in breathing disruptions after 3 months of EPAP use. The participants also found the EPAP device easy to wear all night. In another study, more than half of participants experienced a reduction in breathing interruptions and daytime sleepiness after a full year of EPAP use.
EPAP vs CPAP
EPAP and CPAP are medical devices used to treat obstructive sleep apnea. Both treatments create positive pressure to prevent a person’s airway from collapsing during sleep. All devices designed to treat OSA, including CPAP and EPAP, require a prescription in the U.S.
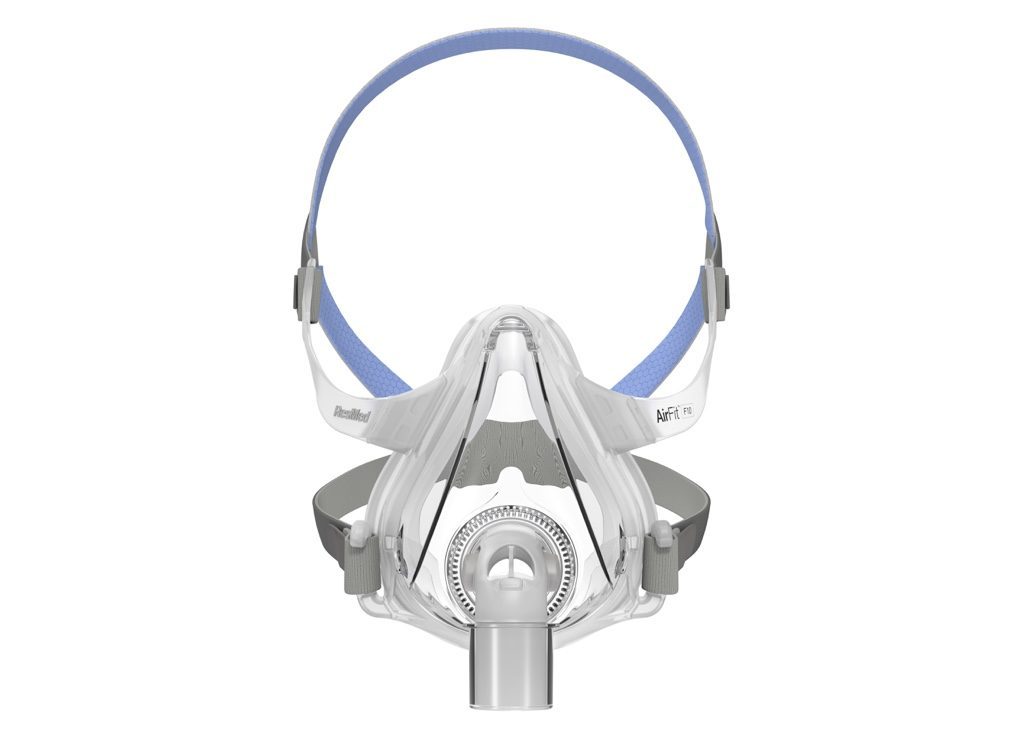
Continuous positive airway pressure keeps the airway open using a machine that pumps air through a hose and into a mask worn over the nose, mouth, or both. A CPAP delivers air at the same rate throughout the night to prevent the airway from collapsing. Some of the costs associated with CPAP are covered by medicare and many private health insurance providers.
In contrast, a nasal EPAP device doesn't require a mask, hose, or machine. Instead, an EPAP device is placed in the nostrils and keeps the airway open by limiting a sleeper’s exhalations. Unlike a CPAP device, EPAP devices do not require electricity or routine maintenance. EPAP devices may not be covered by health insurance providers.
How to Decide which PAP Therapy is Right for You?
If you have been diagnosed with OSA, talk with your doctor or sleep specialist to determine the best treatment option for you. Because nasal EPAP is an emerging technology, additional research is needed to determine the treatment’s effectiveness and appropriate candidates for this alternative to CPAP.
CPAP is a common method of providing positive airway pressure therapy, preferred by many doctors because of its familiarity and proven effectiveness. However, people who have difficulties tolerating CPAP devices may be appropriate candidates for EPAP.
Reasons why people may not tolerate CPAP include:
- Claustrophobia
- Discomfort from CPAP mask
- DIfficulties tolerating air pressure
- Congestion or nasal dryness
More research is needed to compare the effectiveness of EPAP and CPAP therapy. Although some studies have found that CPAP is better than EPAP at reducing the number of breathing interruptions per hour, other studies have found that CPAP is more effective or that both treatments are roughly equal in their ability to improve nighttime breathing.
EPAP therapy may be appropriate for people who cannot tolerate CPAP and who have mild to moderate OSA. Mild OSA is defined as 5 to 14 breathing interruptions per hour, while moderate OSA involves 15 to 29 interruptions each hour. EPAP may not be appropriate for people with severe OSA, who experience 30 or more breathing interruptions per hour.
Medical Disclaimer: This content is for informational purposes and does not constitute medical advice. Please consult a health care provider prior to starting a new treatment or making changes to your treatment plan.