Continuous positive airway pressure (CPAP) machines treat obstructive sleep apnea by directing a stream of pressurized air into the upper airway to prevent breathing from being blocked. Having the appropriate CPAP pressure settings is essential to effectively resolve sleep apnea symptoms.
We cover how CPAP pressure levels are established and what can happen if the pressure is too high or too low. We also review the factors that help determine the required air pressure and when to talk to your doctor about a potential adjustment to your CPAP settings.
Think You May Have Sleep Apnea? Try an At-Home Test

our partner at sleepdoctor.com
Save 45% on your Sleep Test Today
Shop now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
What Should Your CPAP Pressure Be?
Your CPAP pressure level should be tailored to your specific needs. Your doctor or a sleep technician will help determine the lowest amount of pressure necessary to eliminate the breathing disruptions associated with obstructive sleep apnea.
A CPAP’s pressure level is a numeric value measured in centimeters of water (cm H2O). Many CPAP machines can operate at pressures ranging from 4 to 20 cm H2O. While there is considerable variation between individuals, the average CPAP setting is between 8 and 10 cm H2O.
How Is Your CPAP Pressure Level Determined?
The traditional way of establishing CPAP pressure settings is by trying out different pressure levels during an overnight sleep study in a specialized sleep lab.
The process of determining the right pressure level is known as CPAP titration, and the goal of titration is to find the minimal level of pressure required to fully treat obstructive sleep apnea. Your prescribed pressure level can depend on the severity of your symptoms, the type of mask you use, and a range of other factors.
During CPAP titration, you use a CPAP device while sleeping in the laboratory. At first, the pressure level is set very low. A technician then monitors your breathing and gradually increases the pressure until breathing disruptions are resolved.
CPAP titration sometimes happens during the same sleep study that can determine whether you have sleep apnea. In other cases, you may have to return to the sleep lab for a second overnight study.
Experts consider CPAP titration performed during a sleep study to be the most accurate way of finding the optimal CPAP pressure level. In some cases, CPAP pressure levels can be determined at home using an auto-adjusting positive airway pressure (APAP) device.
An APAP machine detects breathing interruptions and automatically increases or decreases air pressure as needed. People with moderate or severe OSA without other respiratory conditions may be presented with this option.
Based on data collected by the device, it may automatically change pressure levels, or your doctor may suggest an update to the settings. In certain instances, the data may indicate a need to return to the sleep lab for another CPAP titration.
How to Set Your CPAP Machine’s Pressure
When you receive a CPAP device, it will usually be pre-programmed to the pressure level recommended by your health care team. You can view the pressure level on the machine’s screen, but you should avoid making any changes to the settings without first consulting with your doctor.
Remember that your CPAP’s pressure has been set in accordance with your specific needs and the severity of your sleep apnea. Making modifications without the guidance of your health care team could interfere with the effectiveness of CPAP therapy.
If you believe that your CPAP pressure needs adjustment, your doctor may be able to suggest changes and guide you through changing the device’s settings. Examples of two changes that may be available on CPAP machines are pressure ramp and pressure relief.
- Pressure ramp: This setting allows for a slow buildup of pressure over a period of around 5 to 45 minutes. The goal of the pressure ramp is to allow you to fall asleep before the highest pressure level sets in.
- Pressure relief: The pressure relief setting enables a small reduction in air pressure when you exhale, which may make breathing more comfortable. However, pressure relief settings are not standard, so it’s important to consult with a doctor to ensure that pressure relief is properly set up on your device.
APAP Pressure Settings
While a CPAP machine provides a fixed level of air pressure, an auto-adjusting positive airway pressure (APAP) device uses sensors to monitor your breathing and then adapts the pressure level to resolve breathing disruptions. APAP is now the most common way to treat obstructive sleep apnea in the U.S.
An APAP device is also sometimes called an auto-titrating PAP because the device itself can find the necessary air pressure level to keep your breathing uninterrupted. In this way, an APAP machine can avoid the need to do CPAP titration in a sleep lab.
When you receive an APAP machine, it is frequently set to a pressure range, such as 5 to 20 cm H2O, and the pressure moves up or down within that range as needed. Sometimes the initial settings will be based on your sleep study. Depending on your circumstances and the data recorded by the APAP device, the doctor can suggest changes to the pressure range.
Side Effects of CPAP Pressure Not Properly Set
Setting the proper pressure level on your CPAP machine is important for increasing the effectiveness of treatment for obstructive sleep apnea. It is also important for reducing side effects from CPAP therapy. There are potential downsides to CPAP pressure that is too high or too low.
When Your CPAP Pressure is Too High
The higher the CPAP pressure level, the more forceful the flow of air will feel when you breathe in or out. Excess pressure can cause multiple unwanted effects.
- Discomfort: Some people experience difficulty when exhaling against higher CPAP air pressure levels, which can make using the CPAP uncomfortable.
- Nasal irritation and congestion: The stream of pressurized air can irritate the inside of the nose and increase nasal congestion. Being congested can make it harder to breathe normally, which may affect CPAP usage.
- Dryness of the nose or mouth: High-pressure airflow through the mask may dry out the inside of the nose or mouth. Most CPAPs now have a built-in humidifier to try to reduce this drying effect.
- Bloating and gas: When using a CPAP, some people swallow pressurized air, which may lead to feeling bloated or gassy.
- Eye irritation: Higher pressure can cause more air to leak out from around an ill-fitting mask. If this occurs, the air may reach the eye and cause dryness or irritation.
These types of side effects of excess air pressure may pose a challenge to sticking with CPAP therapy, which can prevent this treatment from addressing the symptoms of sleep apnea.
CPAP pressures that are too high can also lead to a type of central sleep apnea called complex sleep apnea. If you have concerns about your CPAP pressure being too high, talk with your doctor.
When Your CPAP Pressure is Too Low
If CPAP pressure is too low, then using the device may not effectively keep the airway open during sleep. In this situation, the symptoms of obstructive sleep apnea may continue despite consistent CPAP use. These symptoms can include:
- Frequent and loud snoring
- Gasping, choking, or lapses in breathing
- Waking up unrefreshed
- Daytime sleepiness
- Morning headaches
If CPAP pressure is too low to resolve breathing disruptions during sleep, then there may also be risks of health complications from obstructive sleep apnea such as high blood pressure and other cardiovascular problems.
Factors That Affect CPAP Settings
There is no standard CPAP pressure level that works for everyone. Instead, multiple factors influence the proper pressure level.
- Sleep apnea severity: The CPAP settings are calibrated to resolve all breathing disruptions, so pressure levels must be established to match the severity of sleep apnea.
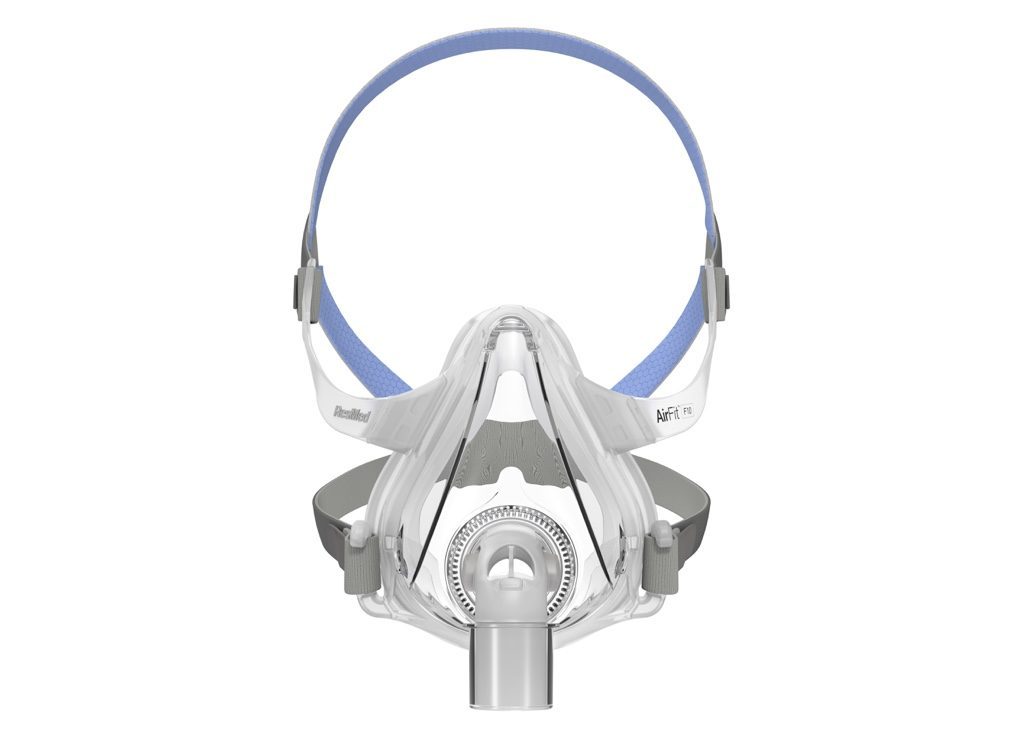
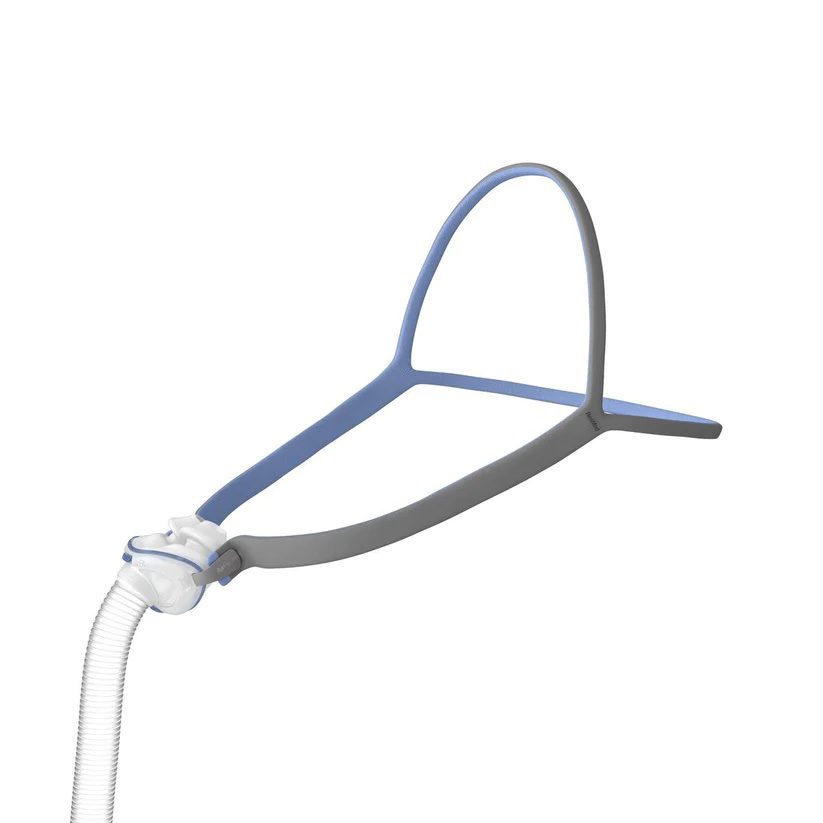
- Mask type: Not all masks can be used to deliver the same amount of pressure, so the kind of mask you use may impact pressure settings. Pressure levels may also need to be adjusted to account for air that leaks out from your mouth or from around your mask.
- Body weight: Having obesity can exacerbate breathing disruptions during sleep, and pressure levels may need to be modified in response to changes in body weight.
- Sleeping position: Sleeping on your back can worsen OSA, and a person’s sleeping position may influence how much air leaks out from around the mask. CPAP pressure is usually configured to eliminate breathing disruptions in every sleeping position.
- Facial anatomy: Pressure levels may need to account for certain aspects of facial anatomy that can impact breathing during sleep and how effectively air from a CPAP can be delivered.
- Use of sedatives or alcohol: Substances that have a sedative effect, including alcohol, may contribute to disrupted breathing. Regular evening use of alcohol or sedatives may require a higher CPAP pressure to adequately treat obstructive sleep apnea.
- Nasal congestion: When the nasal passageways are congested or irritated, it can create added resistance to the stream of air from the CPAP, and air pressure levels may have to be adjusted as a result.
- Altitude: Air pressure is directly affected by altitude, so a CPAP’s pressure may need to be modified based on the location where it is being used. For most devices, though, the settings allow users to automatically make altitude-related adjustments.
Because so many different factors can play a role in finding the proper CPAP settings, it is important to always work with your health care team if you have concerns about CPAP pressure or are interested in making an adjustment to the pressure level.
When to Get Your CPAP Settings Adjusted
While your health care team will work to make your initial CPAP pressure settings as effective as possible, there are times when the pressure level may need to be changed.
In some cases, your doctor will suggest making an adjustment to your CPAP based on their assessment of how well CPAP treatment is working. This may involve reviewing data collected by your CPAP or APAP device that indicates how often you are using it and the frequency of any breathing disruptions during sleep.
You should also talk to your doctor if you notice any issues that may suggest a pressure adjustment is needed, including:
- Discomfort that affects your ability to consistently use your CPAP
- Side effects from CPAP use
- Persistent sleep apnea symptoms like snoring or daytime sleepiness
- Air leaks or a mask with a poor fit
- An increase or decrease in body weight
- Changes in evening alcohol consumption
- Changes to daily medications, especially any sedatives
These issues may not always require a change in pressure levels. Sometimes other steps may be available to troubleshoot CPAP problems and make it easier and more comfortable for you to use your device as intended.
In some situations, your doctor may ask you to do another overnight sleep study in order to more accurately assess your breathing and find the right pressure level.
If it is necessary to change your device’s pressure settings, your health care team will either make those changes for you or provide direct assistance so that you can update the settings on the machine yourself.