A bilevel positive airway pressure machine, also called a BiPAP or BPAP machine, uses two levels of pressurized air to help users breathe properly while sleeping. The machine has one level for inhalation, then switches to the second level for exhalation. BiPAP is a type of positive airway pressure (PAP) therapy that involves the delivery of pressurized air via a hose that connects to a mask.
PAP therapy is the leading treatment option for obstructive sleep apnea (OSA), a condition in which breathing pauses during sleep due to a blockage in the upper airway. The more common form of PAP therapy for OSA is continuous positive airway pressure (CPAP) therapy, which uses a machine with only one air pressure level, but BiPAP is useful for some people with OSA who do not respond well to CPAP.
BiPAP machines are also used by some people with central sleep apnea (CSA) — a condition characterized by pauses in breathing during sleep due to the brain failing to send signals to the muscles that control breathing — as well as other less common breathing disorders.
How Does a BiPAP Machine Work?
BiPAP machines generate pressurized air that is sent through a hose and delivered to the user’s upper airway via a mask. Most BiPAP masks cover the nostrils, nose, or nose and mouth, though other options are available.
The two air pressure levels used by a BiPAP machine are called inspiratory positive airway pressure (IPAP) and expiratory positive airway pressure (EPAP). The IPAP level, which is generally the higher number of the two, is used during inhalation. The machine switches to EPAP when the user exhales.
The difference in pressure settings between IPAP and EPAP aids inhalation while also making it easier to breathe out against the flow of pressurized air. Most BiPAP machines have additional settings that can be used to help regulate breathing patterns.
What Are the Different BiPAP Operating Modes?
Since BiPAP machines are used for a number of conditions, each with its own treatment requirements, they typically have multiple modes of operation to provide different forms of therapy. If your doctor prescribes BiPAP therapy, they will explain which setting is right for you.
BiPAP Modes of Operation
| Spontaneous | A BiPAP machine used in spontaneous mode, or S mode, switches from IPAP to EPAP according to the user’s natural breathing pattern. This mode works well for some people with OSA, though it may be less effective for others, such as those with central sleep apnea. |
| Spontaneous Timed | Spontaneous timed mode, also known as S/T mode, works the same as spontaneous mode unless the machine detects that it has been too long since the user has breathed in. At this point, the machine goes through a programmed IPAP and EPAP cycle to deliver a “backup breath” and facilitate breathing. |
| Timed | Timed mode, or T mode, switches between IPAP and EPAP according to a timed schedule and does not respond to the user’s spontaneous breathing pattern. This setting is used less often than the S or S/T modes, as the difference in timing between ventilation and spontaneous breathing can make breathing more difficult for some people. |
How Are the IPAP and EPAP Pressure Settings Determined?
After a person has been prescribed a BiPAP machine, they must attend a titration study to determine their correct IPAP and EPAP settings.
The titration, which usually occurs at a sleep clinic, involves the person being fitted with both a mask and electrodes before going to sleep. While they sleep, medical professionals use information gathered from the electrodes as they adjust the IPAP and EPAP settings throughout the night to find optimal levels.
After the titration study, the participant’s doctor is given IPAP and EPAP recommendations based on the air pressure required to control their symptoms during the study.
What’s the Difference Between a BiPAP and a CPAP Machine?
BiPAP and CPAP are both forms of positive airway pressure therapy, which uses pressurized air to regulate breathing, but they differ in how they work and when they are usually prescribed.
CPAP machines use a single pressure setting regardless of whether the person is inhaling or exhaling. BiPAP, on the other hand, has two air pressure levels that are set by a clinician and work together to normalize breathing.
Is a BiPAP Machine Right for Me?
While BiPAP is regularly used to treat a number of different conditions, it is often prescribed only after someone has tried CPAP therapy and found it ineffective or too uncomfortable. However, there are some situations when a doctor may prescribe BiPAP therapy before CPAP.
In addition to CPAP and BiPAP, there are other types of PAP machines that use complex algorithms to determine the most appropriate pressure level from breath to breath.
Other Types of PAP Therapy
| Auto-BiPAP | Automatic BiPAP machines, also called auto-BiPAP, use the clinician’s settings combined with an algorithm to determine the best IPAP and EPAP from breath to breath. Since auto-BiPAP machines use the lowest effective pressure levels for inhalation and exhalation, some people find them more comfortable to use than standard BiPAP machines. Others may find that the changes in air pressure make it more difficult to sleep. |
| APAP | Automatic positive airway pressure (APAP) machines change the air pressure level within a prescribed range depending on the user’s needs. Unlike BiPAP, APAP therapy does not provide two distinct pressure levels for inhalation and exhalation. While some APAP machines have an optional comfort setting called expiratory pressure relief that gently lowers air pressure during exhalation, BiPAP machines allow for a greater difference between inspiratory and expiratory pressure. |
| ASV | Like APAP machines, adaptive servo-ventilation (ASV) machines can adjust air pressure based on a user’s breathing patterns. However, ASV machines are bilevel devices that change air pressure levels according to more sophisticated algorithms, including the ability to force inhalation. Conditions treated with ASV machines include central sleep apnea and Cheyne-Stokes respirations. The latter involves alternating periods of apneic events and hyperventilation. ASV is not recommended for some people with chronic heart failure. |
Sleep-Related Breathing Conditions Treated Using BiPAP Machines
Besides obstructive sleep apnea, BiPAP machines are a treatment option for other less common sleep breathing disorders. BiPAP is used as a first choice of treatment in some situations, while in other cases it may be prescribed after a person has unsuccessfully tried CPAP.
Obstructive Sleep Apnea (OSA)
The most common sleep breathing disorder, OSA is a condition that causes people to experience pauses in breathing during sleep due to an obstruction in their airway. This obstruction is usually caused when muscles and tissues in the throat relax during sleep.
PAP therapy helps treat OSA by using pressurized air to keep the airway open and free of obstructions. Some people with OSA switch from CPAP to BiPAP if they find it difficult to exhale against the CPAP machine’s single pressure level. BiPAP may also be prescribed to people for whom CPAP has been ineffective.
Central Sleep Apnea (CSA)
While people with OSA are trying to breathe past an obstruction, those with CSA frequently stop making an effort to breathe during sleep.
Some people have CSA without a clear reason, called idiopathic OSA. Others get CSA because of another problem, like Cheyne-Stokes breathing. Conditions like muscular dystrophy or long-term use of strong painkillers can also cause CSA.
There are multiple treatment options for CSA, including PAP therapy using a CPAP, BiPAP, or ASV machine. CPAP is considered the first choice for treating CSA, though BiPAP or ASV may be more effective in some cases.
What Are Some Common Side Effects of BiPAP Therapy?
All forms of PAP therapy are associated with side effects. While in most cases these side effects are mild, they can make treatment adherence more difficult. Some people find relief from PAP side effects by using therapy accessories.
Dry Mouth, Nose, and Throat
The pressurized air generated by a BiPAP machine can cause the mouth, nose, sinuses, and throat to dry out. This can cause inflammation, soreness, nose bleeds, and sinus congestion that in some cases can impact the effectiveness of BiPAP therapy.
Warm humidifiers and heated tubes can add moisture to the air, making it easier on the throat and nose. Some BiPAP machines have integrated humidifiers, though external humidifiers are also available.
Mask Discomfort
BiPAP masks can be uncomfortable for some people, particularly new users unaccustomed to wearing one each night. Some people experience physical discomfort due to skin irritation or redness, while others find the mask claustrophobic.
Choosing the right BiPAP mask is the easiest way to prevent mask discomfort, though some people need to try several mask types and models before finding one that works for them. Mask liners, which are made from breathable fabric, can also help prevent irritation or redness.
Depending on your mask type and preferred sleep position, you may find it easier to sleep with a CPAP pillow. These specialized pillows feature cutouts or curves that provide space for a mask and hose.
Is a Prescription Needed for a BiPAP Machine?
PAP machines, including BiPAP machines, can only be purchased with a prescription from a medical provider.
Purchasing a BiPAP machine from a brick-and-mortar location, whether from a sleep specialist or CPAP retailer, requires customers to either have a physical prescription or a digital prescription sent to the retailer by their doctor. Shoppers can also purchase a BiPAP machine online by uploading or faxing their prescription to the retailer.
Does Health Insurance, Medicaid, or Medicare Cover Your BiPAP Machine Costs?
Health insurance, including Medicaid and Medicare, often covers BiPAP machines and their recurring costs. However, this coverage may only be available under specific circumstances. For example, many providers will only cover the costs of a BiPAP machine for OSA if CPAP therapy has already been attempted and shown to be ineffective.
If you are unsure about whether your provider covers BiPAP therapy, or if you don’t know the circumstances under which it’s covered, it is worth reviewing your provider’s literature or contacting them directly for more information.
Can You Use an FSA or HSA Account for a BiPAP Machine?
BiPAP machines are considered medical devices and are eligible for purchase using a flexible spending account (FSA), health savings account (HSA), or health reimbursement arrangement (HRA). Most CPAP retailers allow customers to use their FSA or HSA debit card when making a purchase.
Where Can BiPAP Machines Be Bought?
Sleep specialists, brick-and-mortar CPAP retailers, and online CPAP retailers are all common places to buy a BiPAP machine, and each location has its own benefits and drawbacks.
- Sleep specialist: Many sleep specialists stock a small range of BiPAP machines and accessories. While the prices may be higher, buying from your specialist gives you the opportunity to receive in-depth advice based on your unique needs.
- Brick-and-mortar CPAP retailer: With a larger selection and lower prices than most sleep specialists, brick-and-mortar retailers are a convenient choice for many people who want to bring their machine home the same day they purchase it.
- Online CPAP retailer: Online retailers are a good choice for people who are primarily interested in a large selection and low prices. Many online CPAP retailers offer free shipping, and some have a chat feature where customers can ask questions about their products.
BiPAP Machines
The average BiPAP machine costs between $1,700 and $3,000 depending on its manufacturer and features. BiPAP machines are generally more expensive than CPAP machines due to their advanced features and the more complex algorithms involved.
It’s important to choose a BiPAP machine based on how well it meets your needs. If you are unsure which machine is right for you, your doctor or sleep specialist can help guide you toward an appropriate model.
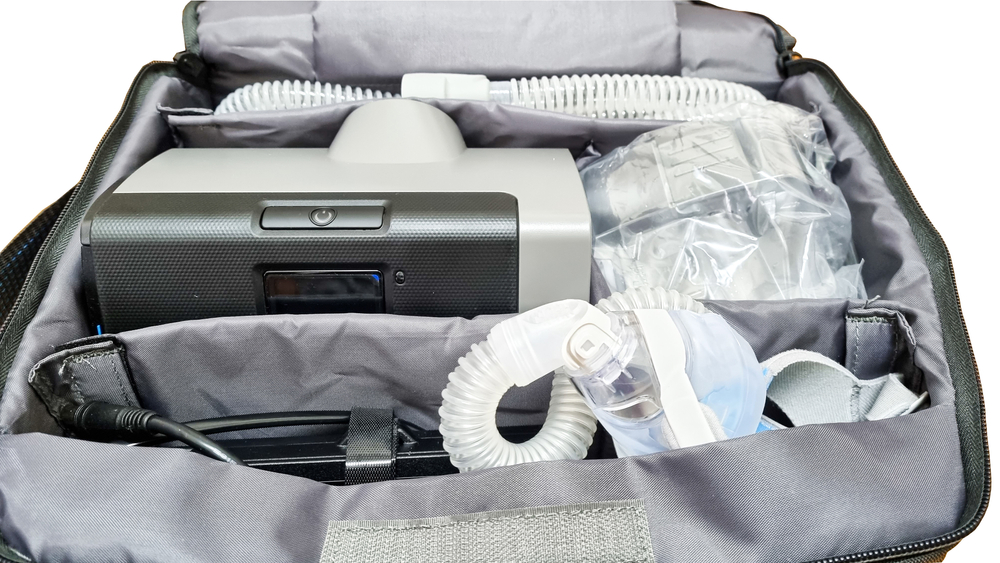
Most BiPAP machines come with tubing, a power cord, at least one air filter, and an instruction manual. BiPAP users are usually responsible for purchasing their mask separately, which allows them to choose the mask that best fits their needs.
Many BiPAP components, such as filters, masks, and hoses, must be replaced on a regular schedule. Cleaning them according to the manufacturer’s instructions can keep them working properly for longer, as well as ensuring your BiPAP machine remains hygienic.
Since BiPAP machines are mechanical devices that can help people breathe, they are considered a type of ventilator. The pressurized air generated by a BiPAP machine is delivered through an external mask, making it a noninvasive form of ventilation. More invasive forms of ventilation used for life support involve intubation, in which air is delivered through a tube that’s inserted into the trachea through the nose or mouth.
Medical Disclaimer: This content is for informational purposes and does not constitute medical advice. Please consult a health care provider prior to starting a new treatment or making changes to your treatment plan.
References
+24 Sources
- Accessed on April 12, 2023. https://www.uptodate.com/contents/obstructive-sleep-apnea-overview-of-management-in-adults
- Accessed on April 12, 2023. https://pubmed.ncbi.nlm.nih.gov/24666419/
- Accessed on April 12, 2023. https://www.ncbi.nlm.nih.gov/books/NBK578199/
- Accessed on April 12, 2023. https://www.ncbi.nlm.nih.gov/books/NBK560916/
- Accessed on April 12, 2023. https://pubmed.ncbi.nlm.nih.gov/26604837/
- Accessed on April 12, 2023. https://pubmed.ncbi.nlm.nih.gov/25902825/
- Accessed on April 12, 2023. https://pubmed.ncbi.nlm.nih.gov/29724743/
- Accessed on April 12, 2023. https://pubmed.ncbi.nlm.nih.gov/32984212/
- Accessed on April 12, 2023. https://pubmed.ncbi.nlm.nih.gov/36116818/
- Accessed on April 12, 2023. https://pubmed.ncbi.nlm.nih.gov/18468315/
- Accessed on April 12, 2023. https://pubmed.ncbi.nlm.nih.gov/32309284/
- Accessed on April 12, 2023. https://www.ncbi.nlm.nih.gov/books/NBK448165/
- Accessed on April 13, 2023. https://aasm.org/special-safety-notice-asv-therapy-for-central-sleep-apnea-patients-with-heart-failure/
- Accessed on April 13, 2023. https://www.uptodate.com/contents/clinical-presentation-and-diagnosis-of-obstructive-sleep-apnea-in-adults
- Accessed on April 13, 2023. https://pubmed.ncbi.nlm.nih.gov/32386695/
- Accessed on April 13, 2023. https://pubmed.ncbi.nlm.nih.gov/35683544/
- Accessed on April 13, 2023. https://www.uptodate.com/contents/central-sleep-apnea-treatment
- Accessed on April 13, 2023. https://pubmed.ncbi.nlm.nih.gov/25988636/
- Accessed on April 13, 2023. https://pubmed.ncbi.nlm.nih.gov/31788413/
- Accessed on April 13, 2023. https://pubmed.ncbi.nlm.nih.gov/30993083/
- Accessed on April 13, 2023. https://www.uptodate.com/contents/treatment-emergent-central-sleep-apnea
- Accessed on April 13, 2023. https://pubmed.ncbi.nlm.nih.gov/33009018/
- Accessed on April 13, 2023. https://pubmed.ncbi.nlm.nih.gov/32212210/
- Accessed on April 13, 2023. https://medlineplus.gov/ency/article/003449.htm