Positive airway pressure (PAP) devices are one of the main ways of treating sleep apnea, a disorder involving interrupted breathing during sleep. Continuous PAP (CPAP), auto-adjusting PAP (APAP), and bilevel PAP (BiPAP), are the three main types of PAP machines.
PAP therapy is often the initial treatment for obstructive sleep apnea (OSA), which occurs when a person’s airway becomes blocked by mouth or throat muscles that relax during sleep.
While CPAP machines are the most commonly used for OSA, knowing about different PAP devices, including CPAPs, APAPs, and BiPAPs, can help you understand the treatment options for sleep apnea and how they work.
What Is a PAP Machine?
A PAP machine delivers pressurized air through a face mask while you sleep to maintain the upper airway open. For people with obstructive sleep apnea, this helps keep the upper airway open to reduce breathing difficulties, snoring, and sleep disruptions.
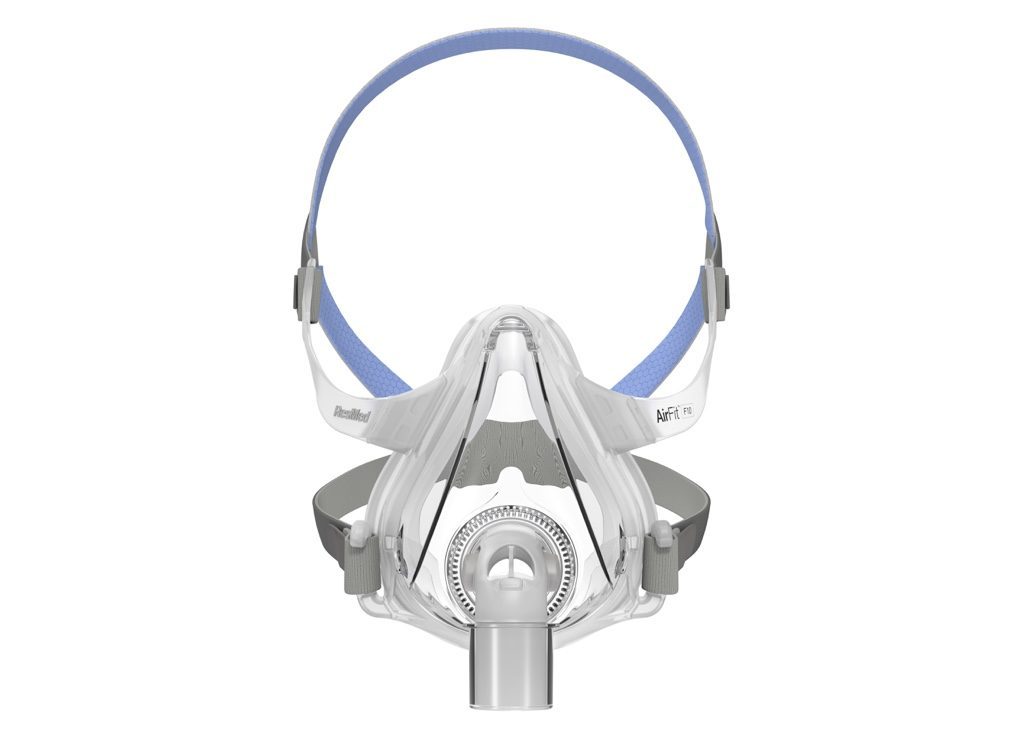
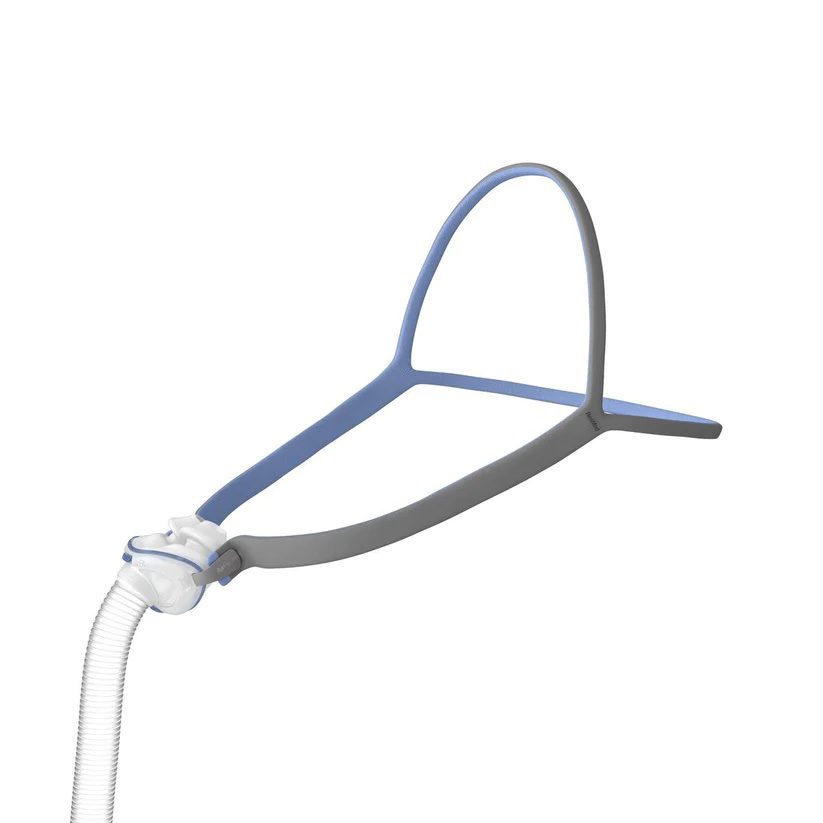
To use a PAP device, a mask is worn over the nose and/or mouth. The mask is connected via a hose to a small machine. The machine pumps air through the hose and mask and into your upper airway while you sleep.
In some cases, PAP machines may also be used to treat central sleep apnea (CSA), which is much less common than OSA. CSA involves interrupted breathing when the brain fails to alert the body’s respiratory muscles to breathe.
Not all PAP devices are the same. Instead, there are multiple types of PAP machines that offer different modes of air pressure.
Continuous Positive Airway Pressure (CPAP)
A CPAP machine provides a steady stream of pressurized air, and the amount of air pressure is the same when you inhale and exhale. Airflow from a CPAP remains constant or fixed throughout a night’s sleep.
Before starting CPAP therapy, it is important to find the right air pressure level. Often, this is determined by a specialist during an overnight sleep study. When you get a CPAP machine to take home, it is already programmed for you. This is known as fixed-level CPAP.
Although CPAP machines usually deliver the same amount of pressure all the time, there are some devices with a “pressure relief” setting that allows for a slight difference between pressure levels when breathing in and out.
Travel CPAP Machines
There are special CPAP machines that are designed for easier travel. These devices are small and lightweight and may be able to run on battery power without always having to be plugged into an outlet.
When flying, a travel CPAP or other PAP device is allowed in carry-on luggage but must be temporarily removed at the TSA security checkpoint for X-ray screening.
Unlike other PAP devices, travel CPAP machines are not usually covered by insurance.
Auto-Adjusting Positive Airway Pressure (APAP)
An automatic or auto-adjusting PAP machine can adjust its air pressure level based on your breathing patterns. Auto-adjusting technology can be added to CPAP machines, which is why it may be called an auto-CPAP machine.
With an APAP device, the pressure level is calculated by the device rather than determined during a sleep study. That pressure level can also be modified by the device on its own. In these ways, APAP therapy is different from fixed-level CPAP.
When you get an APAP machine, the doctor will likely have set an upper and lower limit of air pressure, but software on the device automatically adjusts air pressure within those limits.
For example, if you toss and turn during the night, your ease of breathing may change based on your sleeping position. An APAP machine can detect changes to breathing patterns and increase or decrease air pressure accordingly.
Bilevel Positive Airway Pressure (BiPAP)
BiPAP delivers two air pressure levels, one for inhalation and another for exhalation. This bilevel feature distinguishes BiPAP from CPAP and may be helpful if you have a hard time exhaling against high air pressure, especially when relatively high pressures are needed for your treatment.
The optimal pressure levels for BiPAP therapy are typically established during an overnight sleep study and then programmed into your BiPAP device. These pressure levels prevent lapses in breathing while also reducing snoring and other breathing disruptions.
A BiPAP machine may be configured with one of three different modes.
- Spontaneous mode (S): In this mode, the machine requires the user to initiate each breath before delivering air through the mask. CPAP and APAP machines also require the user to breathe spontaneously.
- Spontaneous timed mode (S/T): This mode has a timer, and if the user does not initiate a breath within a set period of time, then the machine will automatically pump air into the airway. Otherwise, the air is pumped when the user initiates a breath.
- Timed mode (T): In timed mode, the machine does not wait for the user to spontaneously initiate a breath. Instead, the machine pumps air at set intervals.
Another option provided by BiPAP machines is pressure support ventilation (PSV), which helps regulate your breathing rate and the volume of air in each breath. This feature is most often used if you have both OSA and other breathing problems.
BiPAP machines can also use auto-adjusting technology to vary inhalation and exhalation pressure levels throughout the night in response to your breathing patterns. This may be referred to as auto-BiPAP.
Which Type of Machine is Right For You?
The best type of PAP machine for you depends on what type of sleep apnea you have, whether you have other breathing problems, and other factors specific to your situation. A doctor specialized in sleep medicine will help identify which type of machine is right for you.
If you have symptoms of sleep apnea, your doctor will usually recommend a sleep study. If you are diagnosed with OSA, CSA, or another sleep-related breathing disorder, then your doctor will suggest a plan for treatment and may recommend a specific type of PAP machine.
CPAP
CPAP is often the first treatment for people who have OSA and no other conditions that affect their breathing. Typically, the pressure level for the CPAP device is determined during a sleep study.
APAP
An APAP device may be recommended if you have moderate to severe OSA and no other medical conditions that could interrupt breathing. When using an APAP, the pressure levels are determined by the machine rather than by a sleep specialist during an overnight study.
APAP may also be suggested if you:
- Experience discomfort due to high pressures when using a CPAP machine with a fixed level of pressure
- Have frequent changes in your breathing patterns related to your sleeping position, nasal congestion, or use of alcohol or certain medications
- Live far away from a sleep clinic
BiPAP
BiPAP is not typically used as an initial treatment for people with OSA. Instead, it may be used if CPAP therapy is not effective or if you have other breathing problems that arise during sleep as determined by your physician.
BiPAP devices may be recommended for certain types of central sleep apnea, although it should not be used for central sleep apnea associated with heart failure.
Summary of PAP Therapy Machines
It is normal to have questions about PAP therapy machines if you are newly diagnosed with sleep apnea or are in need of new equipment. Your doctor can answer questions about PAP therapy machines. You may also find it helpful to compare the different types of machines.
| Type of PAP Machine | Function | Benefits | Cost |
|---|---|---|---|
| Continuous Positive Airway Pressure (CPAP) | Consistent air pressure level for breathing in and out |
| $500-$1,000 |
| Auto-Adjusting Positive Airway Pressure (APAP) | Auto-adjusting level of air pressure that is generally the same for inhalation and exhalation |
| $1,700-$3,000 |
| Bilevel Positive Airway Pressure (BiPAP) | Provides two levels of air pressure, one for inhalation and a lower one for exhalation |
| $600-$1,600 |
PAP Machines
You will need a prescription from your doctor to obtain any kind of PAP machine. Often, your doctor will ask you to participate in a sleep study in order to make a diagnosis, which can help determine which machine may serve you best. If CPAP, APAP, or BiPAP therapy is suggested, then your doctor will write you a prescription.
Whether you have insurance coverage for PAP therapy depends on your health insurance provider and the details of your policy.
Medicare insurance covers the first 12 weeks of CPAP therapy for people diagnosed with OSA who have a prescription from their doctor. If the CPAP helps improve the symptoms of sleep apnea, then Medicare will continue to cover the cost of CPAP. Both the doctor who writes the prescription and the suppliers of the equipment must be enrolled in Medicare.
Private health insurance providers may fully or partially cover the cost of CPAP machines but not necessarily any replacement parts or accessories. Contact your doctor’s office or your insurance provider to learn more about coverage and any out-of-pocket costs for a CPAP or other PAP therapy.
For some health insurance plans, evidence of consistent use of a PAP device may be required to maintain coverage. Data from the device may be sent to the doctor or insurance provider to demonstrate adherence to the prescribed PAP therapy.
With each type of PAP machine, it is important to find a mask that fits, does not leak air, and is comfortable to wear through the night. Your doctor can usually help select a mask.
You may have some choices when trying to find a mask. Potential customizable parts of masks include:
- Whether it covers the nose, mouth, or both
- The type of cushioning
- Size of the mask
- Whether it has a chin strap to keep the mouth closed
Many PAP devices have other modifiable features. For example, they may have an attached water reservoir and heated humidifier to moisten the air and try to reduce nasal dryness.
Additionally, if you find it hard to fall asleep with high air pressure, it is possible to set a pressure ramp for CPAP, APAP, and BiPAP machines. When a pressure ramp is engaged, the machine delivers lower air pressure for the first 5 to 45 minutes and afterward ramps up to the prescribed levels.