Millions of people in the United States have been prescribed a continuous positive airway pressure (CPAP) device to improve their breathing during sleep. Because COVID-19 can also affect breathing, it is natural that many CPAP users may wonder about the use and maintenance of their CPAP machine during the pandemic.
Given the health benefits of CPAP therapy for obstructive sleep apnea (OSA), it is often advisable to keep using a CPAP even after getting sick with COVID-19. However, any CPAP user who has COVID-19 should talk with their doctor to review the pros and cons of continuing to wear a CPAP in their specific case.
Should You Keep Using a CPAP if You Have COVID-19?
If you use a CPAP machine for obstructive sleep apnea and have COVID-19, you should consult with your doctor about whether to continue using your CPAP while you are sick. In many cases, you can keep using a CPAP device while taking precautions to decrease the risk of spreading the virus to others in your home.
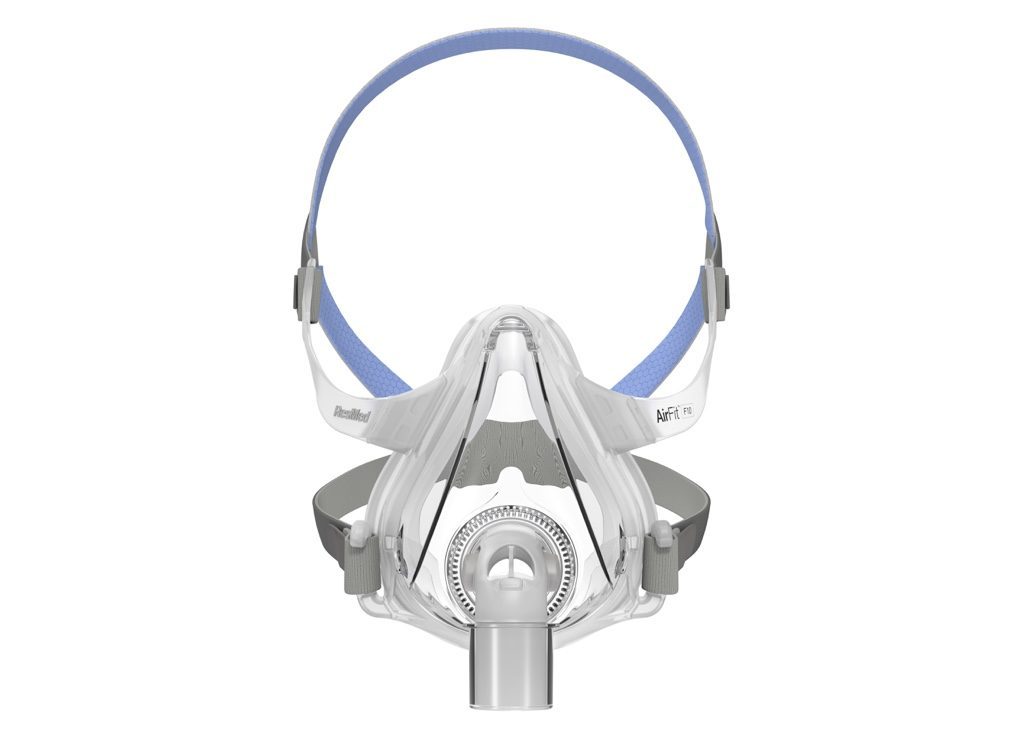
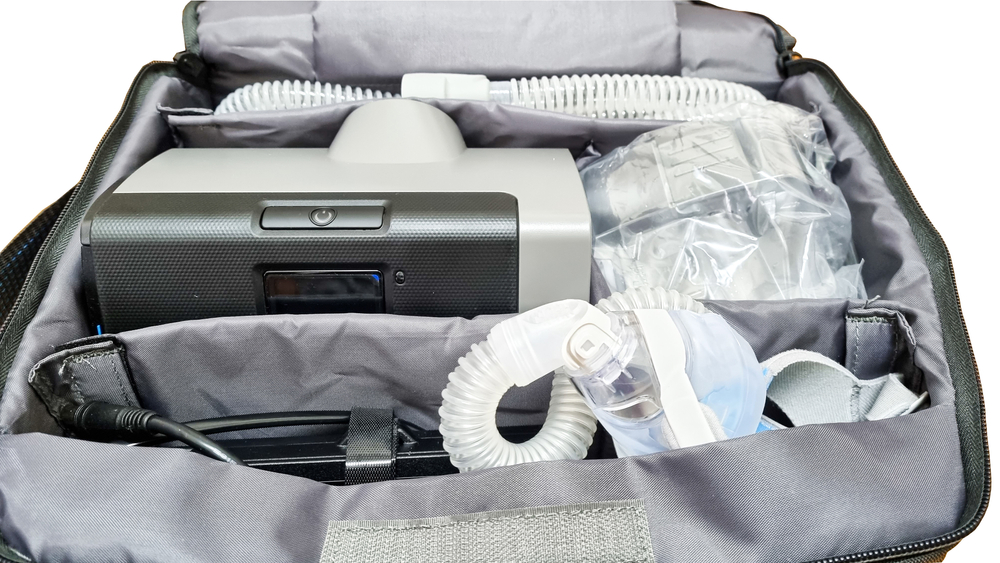
CPAP therapy is one of the most common and effective treatments for obstructive sleep apnea. With a constant stream of pressurized air, a CPAP machine can prevent the upper airway from collapsing during sleep. When used consistently, a CPAP can enhance sleep and prevent health problems linked to OSA.
It is not known whether using a CPAP carries a higher risk of transmitting COVID-19 to other people. While it is possible that a CPAP machine could leak air and spread virus-containing aerosols, evidence to date shows that CPAP machines may spread less of the virus than activities like breathing, speaking, or coughing.
Several factors influence the potential benefits and downsides of using a CPAP for obstructive sleep apnea when you have COVID-19. These factors can be discussed with your doctor to determine the best plan for you.
- The severity of obstructive sleep apnea: You may have a greater need to keep using a CPAP machine if you have more significant breathing disruptions from OSA.
- Potential health complications: Stopping CPAP use may create health risks, including a higher likelihood of cardiovascular problems and car accidents from excessive daytime sleepiness. Your doctor can help you understand the specific risks of pausing CPAP therapy in your case.
- Contact with others in your household: Concerns about spreading COVID-19 may vary based on how much close contact you have with other people and whether anyone in your home is at high risk of severe COVID-19.
- Other available OSA treatments: In some cases, you may be able to take other steps to prevent breathing disruptions during sleep, such as sleeping on your side instead of your back or using an oral appliance prescribed by a doctor.
Though more research is needed, some evidence suggests that continuing to use a CPAP machine for OSA may help decrease the risk of developing severe COVID-19. A CPAP machine can also boost your sleep quality, which promotes a healthier immune system.
If you decide to keep using a CPAP when you have COVID, there are several steps that you can take to best protect yourself and everyone in your home.
- Keep your CPAP clean: Germs can collect in a dirty CPAP, so you want to make sure to closely follow all of the manufacturer instructions about the correct methods to clean your machine and how often it should be cleaned.
- Take precautions: When you have COVID, it’s best to isolate yourself as much as possible to decrease the ability of the virus to spread to others. For example, you can sleep in a separate room when using your CPAP device. During waking hours, wear a mask and follow other precautions suggested by the CDC and your doctor.
- Track your symptoms: Most people have only mild symptoms of COVID-19, but you should be proactive about getting medical attention if your symptoms get worse.
Even if you choose not to keep using a CPAP machine, you should keep a close eye on your symptoms and take steps to limit the risk of transmitting the virus to other people, including by sleeping in a separate room. Carefully follow any advice from your doctor about alternative treatments to reduce breathing disruptions from OSA.
Does Sleep Apnea Increase Your Risk for COVID-19?
Obstructive sleep apnea has not been shown to increase your risk of getting COVID-19. However, some evidence suggests that a COVID-19 infection is more likely to become severe if you have untreated OSA.
COVID-19 is caused by a virus that is transmitted mainly through the air, especially in enclosed spaces or when in close contact with other people. Experts have not identified any direct link between having OSA and contracting COVID-19. Without treatment, though, OSA can hinder sleep, which may impair your immune system and ability to fend off viral infections.
Some evidence has found a link between having OSA and being hospitalized for COVID-19 or developing severe symptoms, but other studies have found no clear connection. Because of the possibility that OSA could affect the progression of COVID-19, your doctor may ask about your symptoms of OSA if you have been diagnosed with COVID-19.
Does Sleep Apnea Increase Your Risk of Long COVID?
Experts are still learning about the long-term effects of COVID-19, but evidence suggests that untreated obstructive sleep apnea may increase the risk of having lasting health problems after COVID-19.
After initially being infected with COVID-19, symptoms may continue for a month or longer. Sometimes new symptoms will arise even after a month or more has passed. These are known as post-COVID conditions or long COVID.
Long COVID is estimated to affect around 1 out of every 16 people who get COVID-19. It can involve a wide range of symptoms, including breathing problems, fatigue, and difficulty thinking. Sleeping problems are another complaint of many people with long COVID.
Without treatment, OSA can interfere with sleep, increase inflammation, and affect the body’s oxygen levels, which may contribute to symptoms linked to long COVID. That said, more research is needed to establish the specific causes of post-COVID conditions and whether obstructive sleep apnea affects a person’s risk of long COVID.
Is CPAP a Treatment for COVID-19?
Separate from their role in treating obstructive sleep apnea, CPAP machines can be adapted to provide oxygen therapy to people with severe COVID-19.
When COVID-19 symptoms are severe, a person may struggle to breathe properly and get enough oxygen. As a result, they may need medical care that helps their lungs get the oxygen they need.
CPAP machines provide a constant flow of air into the upper airway through a mask worn on the face. With the addition of an oxygen therapy device like an oxygen tank, a CPAP machine becomes a non-invasive method of delivering oxygen to the lungs and counteracting the breathing problems caused by severe COVID-19.
It is important to point out that a CPAP machine with an added oxygen tank can be used to provide oxygen to people with severe COVID-19 regardless of whether they have OSA. While CPAP therapy for OSA is only used when sleeping, CPAP treatment for COVID-19 can be applied while a person is awake.
What’s the Difference Between CPAP Machines and Ventilators?
CPAP machines are different from mechanical ventilators. While both can provide breathing support, CPAPs are non-invasive and deliver pressurized air through a mask. In contrast, a mechanical ventilator pumps air to the lungs through a tube that is placed directly into the windpipe.
A mechanical ventilator is typically used to breathe for someone who cannot breathe on their own. Mechanical ventilation is invasive because it requires inserting a tube into the airway through the mouth, neck, or nose.
Doctors may recommend breathing support if a person with COVID-19 is not getting enough oxygen on their own. Non-invasive ventilation may be an option if their oxygen needs are low or moderate. More severe breathing problems may require mechanical ventilation.
In some cases, doctors may first try non-invasive ventilation for people with severe COVID-19 and then switch to mechanical ventilation if their condition doesn’t improve.