In the United States, it is estimated that between 10% and 30% of adults have obstructive sleep apnea, a disorder which causes repeated pauses in breathing during sleep.
Continuous positive airway pressure (CPAP) therapy is one of the most common ways of treating sleep apnea. To get the most out of CPAP therapy, it may be helpful to know how CPAP machines work, how they can help people with sleep-related breathing problems, and how to troubleshoot some of the challenges that may arise when using a CPAP machine.
What Is a CPAP Machine?
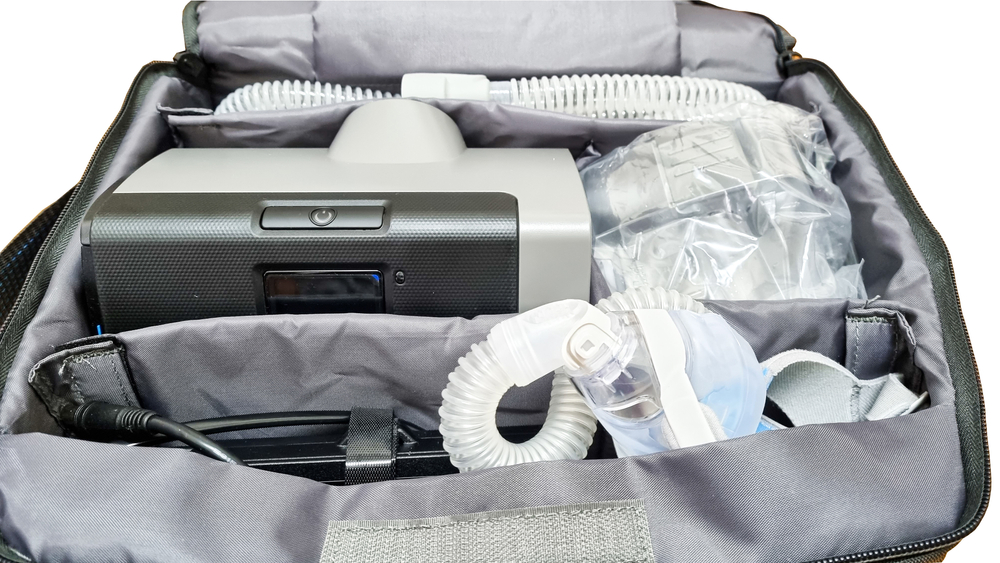
A CPAP machine is a medical device that uses a stream of pressurized air to keep a person’s airway open and encourage stable breathing as they sleep. Air is pressurized in the CPAP machine and pumped through a hose into a mask that is worn on the face.
CPAP therapy is often used as a treatment for obstructive sleep apnea (OSA), a disorder in which the airway narrows or collapses during sleep. CPAP machines are also used to treat other conditions that interfere with breathing.
Components of CPAP Machines
Although there are many different brands and models, CPAP devices have certain standard components.
- Machine: The machine includes controls for operating the device as well as a motor that generates the stream of pressurized air.
- Air filter: This component filters the air generated by the CPAP machine.
- Hose: A long tube connects directly to the CPAP machine and carries air to the mask.
- Mask: The mask delivers the pressurized air into the nose and/or mouth so that the airway is gently stented in an open position for normal breathing during sleep. it can hold the airway open. There are many styles of CPAP masks, and they typically include straps to hold the mask in place.
- Humidifier: Most any CPAP devices have a heated humidifier that uses water from an attached reservoir to add moisture to the airflow. The humidifier is generally used to reduce discomfort from dryness in the nose or mouth caused by the stream of pressurized air. The humidification may be adjusted up or down for comfort or the CPAP user may elect to turn it off.
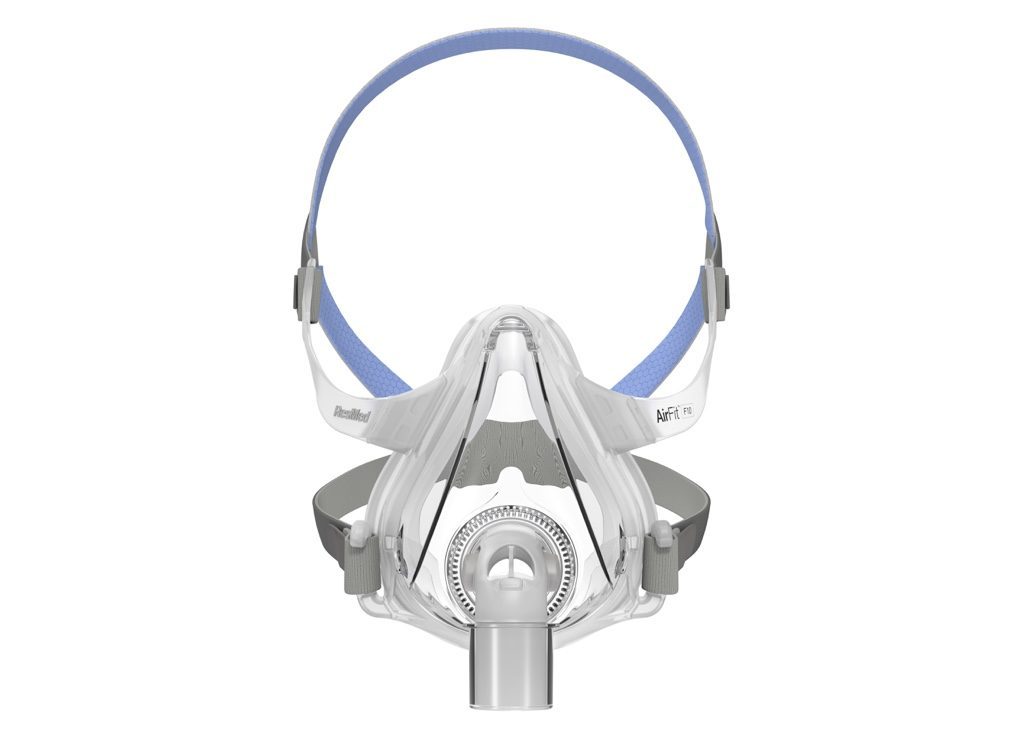
Types of CPAP Masks
Before using CPAP, a doctor or sleep specialist can help you select a mask. There are several different types of masks available.
- Nasal masks: A nasal mask fits around the perimeter of the noses and conducts the pressurized air through the nasal passages.
- Nasal pillows or nasal cradle masks: Instead of going over the nose, a nasal pillow mask or nasal cradle mask sits under the nose and above the upper lip. Nasal pillow masks may have two flexible silicone prongs that seal just inside the rim of each nostril to deliver the pressurized air from the CPAP machine. A nasal cradle mask sits at the base of the nose, with a flexible silicone opening that seals around the nostril openings to conduct air into the nasal cavity.
- Full face mask: This kind of mask goes over the majority of the face and is only used in rare situations.
- Oronasal mask: This type of mask goes over both the mouth and the nose. Often, an oronasal mask covers an area from the bridge of the nose to the bottom of the mouth. Some oronasal masks go over the mouth while using a nasal pillow to deliver air through the nose.
A CPAP mask needs to fit properly against the face so that there are no air leaks. In addition, a mask needs to be comfortable enough that it can be used night after night. Different types of straps and cushions are available to help hold the mask in place and make it more comfortable to wear.
The best CPAP mask for any individual is the one that offers a combination of performance and comfort. Several factors can determine the optimal type and model of mask.
- Facial features: A mask needs to create a seal when held against the face, and finding the right fit can vary based on the size and shape of a person’s facial features. In addition, facial hair may affect the fit of the mask.
- Required pressure: The amount of air pressure can help determine the choice of mask. For example, nasal pillow masks or nasal cradle masks may not be compatible with high air pressure levels.
- How someone breathes: Whether someone tends to breathe through their nose or mouth can influence the right type of mask for their CPAP.
- Individual preference: Comfort is subjective, so individual perceptions of how well a mask fits can play a role in choosing a mask
It is normal for there to be a period of trial and error to find the mask that is the best match for each person’s situation.
Benefits of CPAP Machines
Regular use of a CPAP machine can often reduce or resolve symptoms of obstructive sleep apnea, improving sleep and a patient’s quality of life.
Specific benefits that may come from consistent CPAP use include:
- Reduced snoring
- More consistent breathing during sleep
- Less daytime sleepiness
- Healthier blood pressure
- Improved focus and memory
- Enhanced mood
- Better sleep for a bed partner
- Fewer morning headaches
In most cases, it takes several weeks to notice these benefits, but some people find that their sleep improves almost immediately after starting CPAP therapy.
Side Effects of CPAP Machines
CPAP therapy can provide important health benefits, but it can also cause side effects. For many people, getting accustomed to sleeping with a CPAP machine can be challenging. It often takes days or weeks to get used to using a CPAP machine through the night.
Some side effects that may arise when using CPAP therapy include:
- Discomfort from the mask or stream of pressurized air
- Nasal congestion, dryness, irritation, or nosebleeds
- Claustrophobia or anxiety when wearing the CPAP mask
- Dry mouth
- Skin irritation, especially around the mouth and nose
- Chest muscle discomfort
- Eye irritation
In many cases, practical steps or adjustments of CPAP settings can resolve these side effects and make nightly CPAP use significantly more comfortable. Anyone who experiences one or more of these issues should work closely with their health care team to improve their experience with CPAP therapy.
Tips for Using a CPAP Machine
When getting started with CPAP therapy, several general tips may make the adjustment process smoother.
- Get informed: Seeking out quality information can resolve many common questions about using a CPAP machine. Health care providers can often provide pamphlets, reputable online resources, or videos that cover practical information about using a CPAP device.
- Work with a doctor: Staying in touch with the health care team in the first weeks of using CPAP can help resolve common challenges. A doctor may offer suggestions for different masks or modifications to CPAP settings that can ease the transition to regular use.
- Be patient: The mask or airflow may feel uncomfortable or make it hard to sleep at first, and it is normal for it to take time to adjust to using a CPAP machine. Despite these difficulties, using the CPAP nightly for as long as you’re able can speed up the process of acclimating to the device.
High CPAP Pressure
For some people, the constant flow of pressurized air can be uncomfortable. Several approaches can help manage a feeling of excess air pressure.
- Ramp function: CPAP devices may offer a ramp feature that starts the night with a lower pressure level that builds up over time. This allows a person to fall asleep while the air pressure is lower and less bothersome.
- Pressure relief setting: Some CPAP devices include a pressure relief setting that slightly decreases the air pressure when a person exhales.
- Changing devices: If the steady air pressure of a CPAP is not tolerable, a doctor may consider switching to a type of PAP device that has more variability in the pressure levels.
Having the right pressure level is important to properly treating obstructive sleep apnea, so it is important to work with a doctor before making any changes to a CPAP device’s pressure settings.
Uncomfortable CPAP Mask
It can be hard to find a CPAP mask that can be worn comfortably throughout the night. For people struggling with their mask, it can be helpful to work with their health care team to consider other mask options.
Masks come in many different styles and shapes. The placement of the straps and type of padding can affect how it feels. With so many options available, many people will need to try out a number of masks before finding the one that works best for them.
Waking Up With a Dry Nose
When pressurized air is delivered through the nose, it can cause the inside of the nostrils to dry out, especially for people who live in arid climates or have their home heating system turned on.
In most cases, using a CPAP machine’s heated humidifier can decrease nasal dryness. Most devices allow for the degree of heated humidification to be adjusted through settings on the CPAP device itself.
Waking Up With a Stuffy Nose
CPAP masks may contribute to nasal congestion. Prescription medications may help with this congestion, and for some people, the problem may be resolved by switching to a mask that covers both the mouth and nose.
Claustrophobia While Wearing a CPAP Mask
A few different solutions may help if wearing the CPAP mask creates feelings of claustrophobia.
- Mask desensitization: This approach involves putting on the mask during waking hours and practicing while doing something relaxing. The amount of time wearing the mask should be minimal at first and then gradually increase as a person gets acclimated, eventually using the CPAP mask through the night. Be sure to disconnect the CPAP tubing from the mask if you are practicing without the machine on.
- Switching masks: The feeling of claustrophobia may be reduced by changing to a smaller mask or one that has a different profile on the face.
- Relaxation exercises: Learning and practicing relaxation techniques may decrease the anxiety that can come from putting on the mask. Activities such as journaling, meditation, listening to music, or stretching before bed can promote a calm state of mind that enhances sleep quality.
Waking Up With Dry Mouth
Mouth breathing can lead to dry mouth in people who use nasal CPAPs, and this problem may be addressed by using a chin strap that keeps the mouth closed during sleep. People using a full face or an oronasal mask can try using the heated humidifier or turning up the humidifier setting on their CPAP machine to reduce dry mouth.
CPAP Air Leaks
Air leaks occur when the pressurized air from the CPAP does not reach the airway at the back of the throat. This may occur if the mask does not create a tight seal on the face or if a person breathes through their mouth while using a nasal CPAP.
When air leaks occur, they can be addressed by changing the type or shape of the mask. People using a nasal mask can try using a mask with a chin strap that prevents the mouth from opening during the night.
Facial Hair Interfering With CPAP Mask
Tips for people whose facial hair is affecting the fit of a CPAP mask include:
- Switching to a mask with a different shape
- Using a different kind of mask, such as a nasal pillow mask
- Trimming or shaving facial hair
- Using a cloth mask liner or a mask with a memory foam cushion
CPAP Mask Irritating Skin
If a mask or its straps are pressing too firmly against the face, it may cause skin irritation. Dirty masks or old masks may also cause inflammation, skin breakouts, or sensitivity. CPAP masks should not cause skin breakdown or sores on the face or scalp. Practical steps to reduce skin problems from a CPAP mask include:
- Cleaning the mask regularly
- Adjusting straps to avoid having the mask too tight or too loose
- Switching to a different type or size of mask
- Trying one or more types of padding or cushions to reduce pressure on the skin
CPAP Noise
Although modern CPAP devices have become quieter, the noise may be bothersome to some people or their bed partner. Keeping the machine under the bed, adjusting the machine’s alarm settings, adjusting the mask, or wearing earplugs can often decrease noise disruptions.
If noise continues to be a problem, a doctor can help address whether there is a problem with the CPAP machine or whether another model of CPAP can offer quieter performance.
CPAP Cleaning and Maintenance
CPAP devices usually come with specific instructions for cleaning and maintenance, and it is important to follow these directions and any guidance given by the doctor.
Some parts of the CPAP, such as the mask, may need to be cleaned daily, while other parts may need a thorough cleaning and disinfecting on a weekly basis.
In addition, it is important to watch for wear and tear of CPAP components and to replace them when necessary. Masks, straps, and hoses should be replaced periodically based on the manufacturer’s instructions. These items should also be discarded if the material becomes noticeably dirty or damaged.
Comparing CPAP, APAP, and BiPAP
There are several kinds of positive airway pressure (PAP) therapy. Important differences between them relate to how these devices deliver pressurized air to keep the airway open.
- Continuous positive airway pressure (CPAP): A CPAP machine uses a consistent level of air pressure that is the same for inhaling and exhaling.
- Bilevel positive airway pressure (BiPAP or BPAP): A BiPAP machine has two pressure levels, one for when a person inhales and another for when they exhale.
- Auto-titrating positive airway pressure (APAP): Sometimes called an adjustable PAP, or auto-CPAP, these devices can automatically modify pressure levels in response to a person’s breathing. In most cases, that pressure level is the same for both inhalation and exhalation.
For most people with obstructive sleep apnea, CPAP is recommended as the initial treatment. However, if CPAP is not effective or if someone has certain lung diseases or other coexisting health conditions, a different type of PAP device may be prescribed.
A doctor or sleep specialist can discuss the pros and cons of CPAP, BiPAP, and APAP for any specific person.
Talking to Your Doctor About CPAP Therapy
CPAP therapy must be prescribed by a doctor. A doctor or sleep specialist may help select a device, determine the right pressure level, suggest certain settings, and recommend a type of mask. During this process, patients can communicate any preferences they have about specific components of their CPAP setup, including the mask.
When beginning CPAP therapy, it is critical to stay in regular contact with the doctor about any problems or challenges that arise. In many cases, the doctor can suggest strategies to manage or overcome difficulties so that the device can be used every night to treat sleep apnea.
Over time, patients should continue to check in with the doctor about how their CPAP treatment is going and raise any new issues that may have developed. The doctor may use data collected by the CPAP machine to make sure that the mask and device are functioning properly and to see how well the treatment is working.
CPAP Therapy
Still have questions?
Sleep apnea products can be confusing. If you need individualized assistance, send us an email at [email protected] with your questions and we'll help find the best fit for you.