Positive airway pressure (PAP) machines are one of the main ways of treating sleep apnea, a disorder involving interrupted breathing during sleep. Continuous PAP (CPAP), auto-adjusting PAP (APAP), and bilevel PAP (BiPAP), are the three main types of PAP machines, but there are also travel CPAP machines, expiratory positive airway pressure (EPAP) devices, and adaptive servo-ventilation (ASV) machines.
PAP therapy is often the initial treatment for obstructive sleep apnea (OSA), which occurs when a person’s airway becomes blocked by mouth or throat muscles that relax during sleep. CPAP machines are the most common treatment for OSA, so knowing about different PAP devices can help you understand the treatment options for sleep apnea and how they work.
Need a Prescription for CPAP? Start Here.

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
PAP Therapy and Types of Machines
A PAP machine delivers pressurized air through a face mask while you sleep to maintain the upper airway open. For people with obstructive sleep apnea, this helps keep the upper airway open to reduce breathing difficulties, snoring, and sleep disruptions.
To use a PAP device, a mask is worn over the nose and/or mouth. The mask is connected via a hose to a small machine. The machine pumps air through the hose and mask and into your upper airway while you sleep.
In some cases, PAP machines may also be used to treat central sleep apnea (CSA), which is much less common than OSA. CSA involves interrupted breathing when the brain fails to alert the body’s respiratory muscles to breathe.
Not all PAP devices are the same. Instead, there are multiple types of PAP machines that offer different modes of air pressure.
| Type of PAP Machine | Function | Benefits | Cost |
|---|---|---|---|
| Continuous Positive Airway Pressure (CPAP) | Consistent air pressure level for breathing in and out |
| $500 to $1,000 |
| Auto-Adjusting Positive Airway Pressure (APAP) | Auto-adjusting level of air pressure that is generally the same for inhalation and exhalation |
| $1,700 to $3,000 |
| Bilevel Positive Airway Pressure (BiPAP) | Provides two levels of air pressure, one for inhalation and a lower one for exhalation |
| $600 to $1,600 |
| Expiratory Positive Airway Pressure (EPAP) | Delivers resistance only during exhalation to keep the airway open |
| $50 to $150 per month (disposable valves, not a one-time device purchase) |
| Adaptive Servo-Ventilation (ASV) | Monitors breathing in real time and adjusts pressure support on a breath-by-breath basis |
| $1,700 to $3,000 |
Continuous Positive Airway Pressure (CPAP)
A CPAP machine provides a steady stream of pressurized air, and the amount of air pressure is the same when you inhale and exhale. Airflow from a CPAP remains constant or fixed throughout a night’s sleep.
Before starting CPAP therapy, it is important to find the right air pressure level. Often, this is determined by a specialist during an overnight sleep study. When you get a CPAP machine to take home, it is already programmed for you. This is known as fixed-level CPAP.
Although CPAP machines usually deliver the same amount of pressure all the time, there are some devices with a “pressure relief” setting that allows for a slight difference between pressure levels when breathing in and out.
Travel CPAP Machines
There are special travel CPAP machines that are designed for easier portability. These devices are small and lightweight and may be able to run on battery power without always having to be plugged into an outlet.
When flying, a travel CPAP or other PAP device is allowed in carry-on luggage but must be temporarily removed at the TSA security checkpoint for X-ray screening.
Unlike other PAP devices, travel CPAP machines are not usually covered by insurance.
Auto-Adjusting Positive Airway Pressure (APAP)
An automatic or auto-adjusting PAP machine can adjust its air pressure level based on your breathing patterns. Auto-adjusting technology can be added to CPAP machines, which is why it may be called an auto-CPAP machine.
With an APAP device, the pressure level is calculated by the device rather than determined during a sleep study. That pressure level can also be modified by the device on its own. In these ways, APAP therapy is different from fixed-level CPAP.
When you get an APAP machine, the doctor will likely have set an upper and lower limit of air pressure, but software on the device automatically adjusts air pressure within those limits.
For example, if you toss and turn during the night, your ease of breathing may change based on your sleeping position. An APAP machine can detect changes to breathing patterns and increase or decrease air pressure accordingly.
Bilevel Positive Airway Pressure (BiPAP)
BiPAP machines deliver two air pressure levels, one for inhalation and another for exhalation. This bilevel feature distinguishes BiPAP from CPAP and may be helpful if you have a hard time exhaling against high air pressure, especially when relatively high pressures are needed for your treatment.
The optimal pressure levels for BiPAP therapy are typically established during an overnight sleep study and then programmed into your BiPAP device. These pressure levels prevent lapses in breathing while also reducing snoring and other breathing disruptions.
A BiPAP machine may be configured with one of three different modes.
- Spontaneous mode (S): In this mode, the machine requires the user to initiate each breath before delivering air through the mask. CPAP and APAP machines also require the user to breathe spontaneously.
- Spontaneous timed mode (S/T): This mode has a timer, and if the user does not initiate a breath within a set period of time, then the machine will automatically pump air into the airway. Otherwise, the air is pumped when the user initiates a breath.
- Timed mode (T): In timed mode, the machine does not wait for the user to spontaneously initiate a breath. Instead, the machine pumps air at set intervals.
Another option provided by BiPAP machines is pressure support ventilation (PSV), which helps regulate your breathing rate and the volume of air in each breath. This feature is most often used if you have both OSA and other breathing problems.
BiPAP machines can also use auto-adjusting technology to vary inhalation and exhalation pressure levels throughout the night in response to your breathing patterns. This may be referred to as auto-BiPAP.
Expiratory Positive Airway Pressure (EPAP)
Expiratory positive airway pressure (EPAP) is a simpler, less invasive form of sleep apnea therapy that provides resistance only during exhalation. Unlike CPAP, which delivers continuous airflow, EPAP devices allow you to breathe in normally but create back pressure when you breathe out. This back pressure helps keep the airway open by preventing soft tissues in the throat from collapsing during sleep.
EPAP is typically delivered through small, disposable valves that fit over the nostrils—making it lightweight, travel-friendly, and easier to use for people who can’t tolerate traditional CPAP machines. While EPAP is not as effective for everyone—especially those with moderate to severe obstructive sleep apnea—it may be a good option for people with mild sleep apnea or those who struggle with CPAP compliance.
Adaptive Servo-Ventilation (ASV)
Adaptive servo-ventilation (ASV) is an advanced form of positive airway pressure therapy designed primarily for treating central sleep apnea (CSA) and complex sleep apnea syndromes. Unlike standard CPAP or BiPAP, ASV continuously monitors your breathing patterns in real time and adjusts pressure support on a breath-by-breath basis.
It delivers just enough pressure to stabilize breathing during periods of irregular or paused respiration, making it especially effective for individuals whose apnea isn’t caused by airway blockage but by a failure of the brain to send proper signals to breathe. ASV machines provide a set baseline pressure to keep the airway open and vary the inspiratory support as needed to maintain a normal breathing rhythm.
Because of its high level of responsiveness and precision, ASV is typically recommended for patients with central sleep apnea related to conditions like Cheyne-Stokes respiration or those who develop CSA after using CPAP therapy.
How to Decide Which Type of Machine Is Right for You
The best type of PAP machine for you depends on what type of sleep apnea you have, whether you have other breathing problems, and other factors specific to your situation. A doctor specialized in sleep medicine will help identify which type of machine is right for you.
If you have symptoms of sleep apnea, your doctor will usually recommend a sleep study. If you are diagnosed with OSA, CSA, or another sleep-related breathing disorder, then your doctor will suggest a plan for treatment and may recommend a specific type of PAP machine.
CPAP
CPAP is often the first treatment for people who have OSA and no other conditions that affect their breathing. Typically, the pressure level for the CPAP device is determined during a sleep study.
APAP
An APAP device may be recommended if you have moderate to severe OSA and no other medical conditions that could interrupt breathing. When using an APAP, the pressure levels are determined by the machine rather than by a sleep specialist during an overnight study.
APAP may also be suggested if you:
- Experience discomfort due to high pressures when using a CPAP machine with a fixed level of pressure
- Have frequent changes in your breathing patterns related to your sleeping position, nasal congestion, or use of alcohol or certain medications
- Live far away from a sleep clinic
BiPAP
BiPAP is not typically used as an initial treatment for people with OSA. Instead, it may be used if CPAP therapy is not effective or if you have other breathing problems that arise during sleep as determined by your physician.
BiPAP devices may be recommended for certain types of central sleep apnea, although it should not be used for central sleep apnea associated with heart failure.
EPAP
EPAP devices are typically small, disposable, and easy to use, making them a good option for people with mild OSA or those who can’t tolerate traditional CPAP machines. EPAP may not be as effective for people with moderate to severe apnea.
ASV
ASV is typically used to treat central sleep apnea and complex sleep apnea. It's often recommended for people who develop central sleep apnea after using CPAP or for those with conditions like Cheyne-Stokes respiration.
Frequently Asked Questions
You will need a prescription from your doctor to obtain any kind of PAP machine. Often, your doctor will ask you to participate in a sleep study in order to make a diagnosis, which can help determine which machine may serve you best. If CPAP, APAP, or BiPAP therapy is suggested, then your doctor will write you a prescription.
Whether you have insurance coverage for PAP therapy depends on your health insurance provider and the details of your policy.
Medicare insurance covers the first 12 weeks of CPAP therapy for people diagnosed with OSA who have a prescription from their doctor. If the CPAP helps improve the symptoms of sleep apnea, then Medicare will continue to cover the cost of CPAP. Both the doctor who writes the prescription and the suppliers of the equipment must be enrolled in Medicare.
Private health insurance providers may fully or partially cover the cost of CPAP machines but not necessarily any replacement parts or accessories. Contact your doctor’s office or your insurance provider to learn more about coverage and any out-of-pocket costs for a CPAP or other PAP therapy.
For some health insurance plans, evidence of consistent use of a PAP device may be required to maintain coverage. Data from the device may be sent to the doctor or insurance provider to demonstrate adherence to the prescribed PAP therapy.
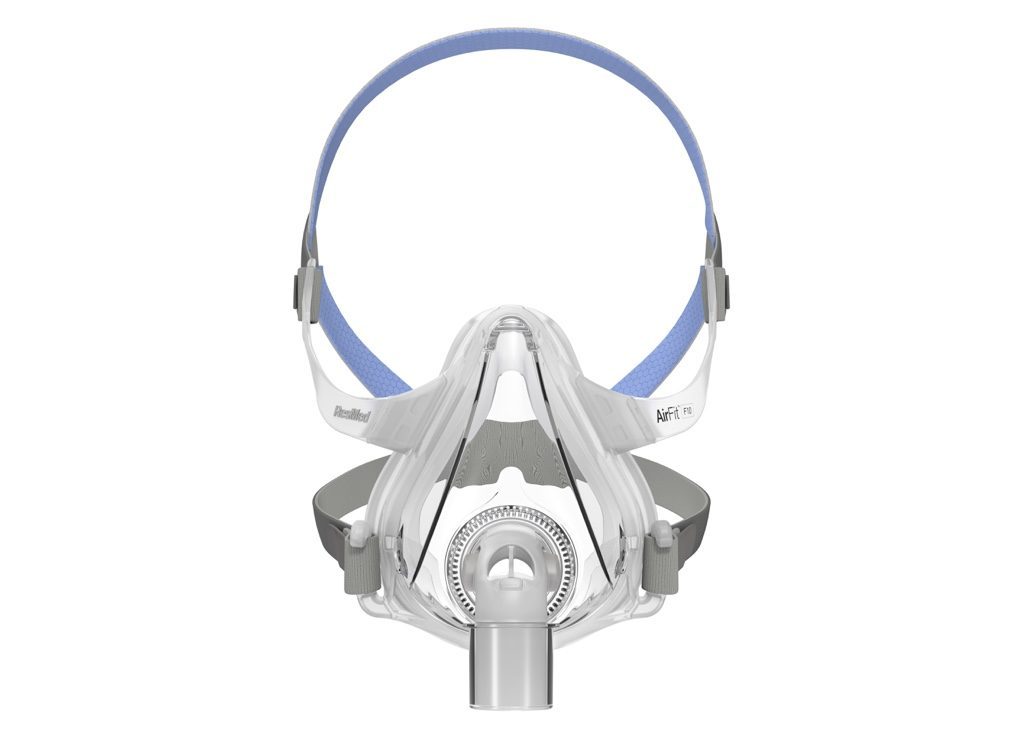
With each type of PAP machine, it is important to find a mask that fits, does not leak air, and is comfortable to wear through the night. Your doctor can usually help select a mask.
You may have some choices when trying to find a mask. Potential customizable parts of masks include:
- Whether it covers the nose, mouth, or both
- The type of cushioning
- Size of the mask
- Whether it has a chin strap to keep the mouth closed
Many PAP devices have other modifiable features. For example, they may have an attached water reservoir and heated humidifier to moisten the air and try to reduce nasal dryness.
Additionally, if you find it hard to fall asleep with high air pressure, it is possible to set a pressure ramp for CPAP, APAP, and BiPAP machines. When a pressure ramp is engaged, the machine delivers lower air pressure for the first 5 to 45 minutes and afterward ramps up to the prescribed levels.
Still have questions?
Sleep apnea products can be confusing. If you need individualized assistance, post your question to the Sleep Doctor forum.