While a cough isn’t the most common CPAP side effect, CPAP therapy can dry out the nose, mouth, and throat — all of which may lead to a cough for some people. Research suggests around 10% of people experience breathing symptoms from CPAP such as congestion, coughing, and sinus problems.
In many cases, a CPAP cough can be resolved with a simple fix like adjusting how the mask fits or following a regular cleaning schedule. However, there are a few other reasons you might be coughing while using CPAP, so it’s important to pinpoint where the cough is coming from.
Think You May Have Sleep Apnea? Try an At-Home Test

our partner at sleepdoctor.com
Save 10% + FREE 2-Day Shipping
Add to Cart“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
Causes of CPAP Cough
In general terms, coughs are the body’s attempt to clear the airway. A CPAP cough may be triggered by factors inherent to the CPAP machine and mask, or it may be due to an underlying condition that needs medical attention.
Dry, Pressurized Air
Cold or dry air irritates the airways and is a common cough trigger. Normally, your nose warms and humidifies the air you breathe in. By contrast, the air that flows from your CPAP device may be dry, cool, and fast-moving. This can irritate the airways and cause nasal congestion, leading you to breathe through your mouth and drying out your mouth in the process. Some people are naturally more sensitive to airway irritation.
CPAP may also affect the mucus system that flushes out unwanted particles, leaving you more sensitive to sinus or nasal inflammation.
Dirty CPAP Mask or Tubing
It’s important to clean your CPAP mask, tubing, and humidifier water chamber on a regular basis to keep out germs. Failure to properly clean your CPAP therapy components can allow mold or bacteria to grow and cause respiratory infections.
Experts warn against using ozone and UV light cleaners to clean your CPAP machine. These may cause headache, breathing difficulties, and coughing. They also void the manufacturer’s warranty for the CPAP.
Mask Leaks
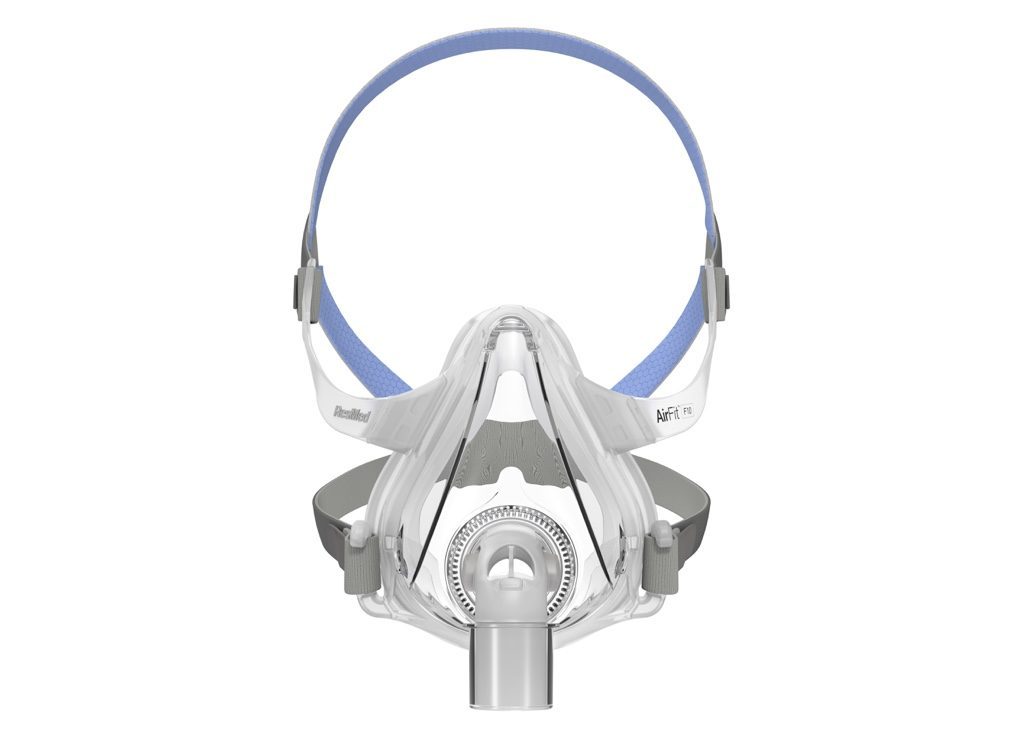
Air leaks may occur due to improperly connected tubing, a poorly fitted mask, or breathing through the mouth when using a nasal CPAP mask. These leaks can cause a stuffy nose and dry mouth, which may exacerbate coughing. Air that escapes may also draw away moisture from the humidifier.
Allergies or Sensitivities
CPAP machines have replaceable filters to ensure allergens like dust mites, dander, and pollen don’t make it into the air you breathe. It’s important to clean or replace these filters regularly, according to the manufacturer’s directions. Otherwise, you may experience coughing from breathing in allergens or irritants like tobacco smoke.
Underlying Respiratory Conditions
Sometimes, a cough may not be caused by CPAP therapy, but rather by an underlying condition that you might not know you have.
Seasonal allergies, asthma, a cold or flu, or other conditions like gastro-esophageal reflux disease (GERD) can cause coughing that happens to be worse when using your CPAP machine. For example, asthma often flares up at night, and heartburn or post-nasal drip from a lingering viral infection both tend to increase when lying down. People who smoke are also likely to have an ongoing cough.
How to Stop CPAP Cough
- Keep your equipment clean: Bacteria and mold can grow in CPAP parts such as the humidifier or tubing, so it’s important to clean them regularly and thoroughly with soap and water to avoid respiratory infections. Instead of reusing the humidifier water, it is best to empty the chamber each morning and refill it with clean distilled water in the evening. Be sure to clean or replace your filters according to the recommended schedule (usually every 2 to 4 weeks for disposable filters) or when they’re visibly dirty.
- Use a humidifier: A heated humidifier is designed to warm and moisten the air before it reaches you, which may help reduce dryness and irritation in the nose and throat. Humidification also clears up congestion in the nasal passages so you don’t have to breathe through your mouth, making it less likely that you’ll have coughing triggered by a dry mouth. The humidifier settings may need to be optimized to prevent oversaturation of the air, another potential source of nasal or sinus congestion and coughing.
- Use heated tubing or tube covers: Using a heated humidifier without heated tubing can cause condensation to form inside the tubes, also known as rainout. This may cause popping or crackling sounds in the tubing as the water collects. If you find the rainout is trickling into your mask, try adjusting the settings on your humidifier or use heated tubing.
- Adjust mask fit: A mask that doesn’t form a snug seal can cause air leaks. Try switching mask styles or using a chinstrap to keep your mouth closed. In some cases, it may be necessary to reach out to your doctor to have the pressure settings turned down.
- Address nasal congestion: A stuffy nose can force you to breathe through your mouth, which dries out your throat. Depending on the cause, you may be able to treat nasal congestion with a nasal saline spray, nasal wash, decongestant, corticosteroid spray, or antihistamines. If obstruction persists, it may be helpful to see an ear, nose, and throat (ENT) specialist.
- Treat underlying respiratory problems: If you’ve tried everything and you’re still coughing, your cough may not be CPAP-related. To get rid of this type of cough, you’ll need to address the root cause. Start by cleaning or removing potential allergen sources in your bedroom such as furniture and bedding. If you have asthma, make sure to use your inhaler as indicated.
When to See a Doctor
You should speak to your doctor if CPAP side effects such as a cough are bothering you, especially if they’re interfering with sleep or making you less likely to use your CPAP therapy. Visit a healthcare professional right away if you have more serious symptoms along with your cough, including:
- Wheezing or trouble breathing
- A “wet cough” that brings up mucus, especially if you’re coughing up colored mucus or blood
- Vomiting from coughing
- A fever or chest pain
- Unexplained weight loss
- Shortness of breath when lying down
- A cough that lasts longer than two weeks
Frequently Asked Questions
It’s important to continue using CPAP therapy as prescribed to reduce the risk of long-term health problems. However, if you have a cough, such as from a cold, that makes CPAP use difficult, you may occasionally need to take a night off. In those cases, sleeping with your head elevated—such as with a wedge pillow in a recliner—may help ease symptoms. If nasal congestion is the main issue, temporarily switching to a full-face mask may allow you to continue CPAP therapy until the congestion improves.
Obstructive sleep apnea often involves snoring, breathing through the mouth, and heartburn, all of which can irritate the throat and potentially contribute to dry mouth and coughing. Coughing that occurs along with OSA may also be due to third factors. For example, anatomical features like large tonsils may contribute to both coughing and OSA. Additionally, OSA is linked to high blood pressure, and blood pressure medications may cause a cough that is worse at night.
Since CPAP therapy blows air into the airway, it’s possible for CPAP therapy to cause a sinus infection if the air contains pathogens. However, the risk is considered low as long as you clean your equipment properly.