At a Glance
A bilevel positive airway pressure machine, also called a BiPAP or BPAP machine, uses two levels of pressurized air to help users breathe properly while sleeping. The machine has one level for inhalation, then switches to the second level for exhalation. BiPAP is a type of positive airway pressure (PAP) therapy that involves the delivery of pressurized air via a hose that connects to a mask.
PAP therapy is the leading treatment for obstructive sleep apnea (OSA), a condition in which breathing pauses during sleep due to a blockage in the upper airway. The more common form of PAP therapy for OSA is continuous positive airway pressure (CPAP) therapy, which uses a machine with only one air pressure level, but BiPAP is useful for some people with OSA who don't respond well to CPAP.
Below, we’ll cover how BiPAP machines work, how they differ from CPAP, and who may benefit from using one.
Need a CPAP Prescription? Start Here

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
How Does a BiPAP Machine Work?
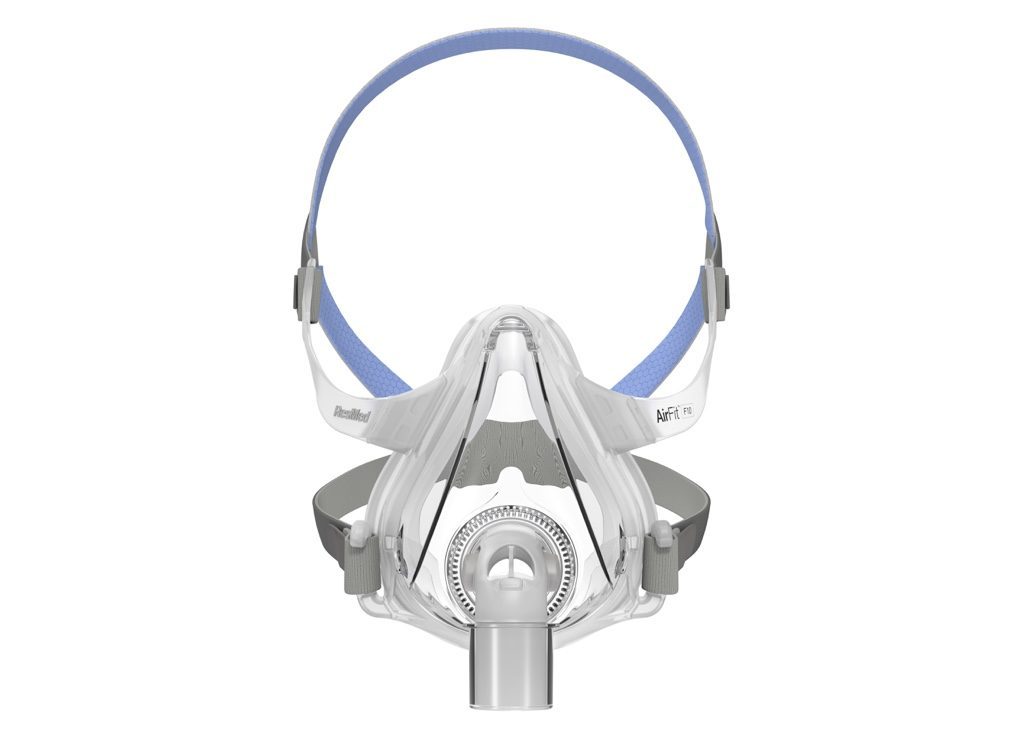
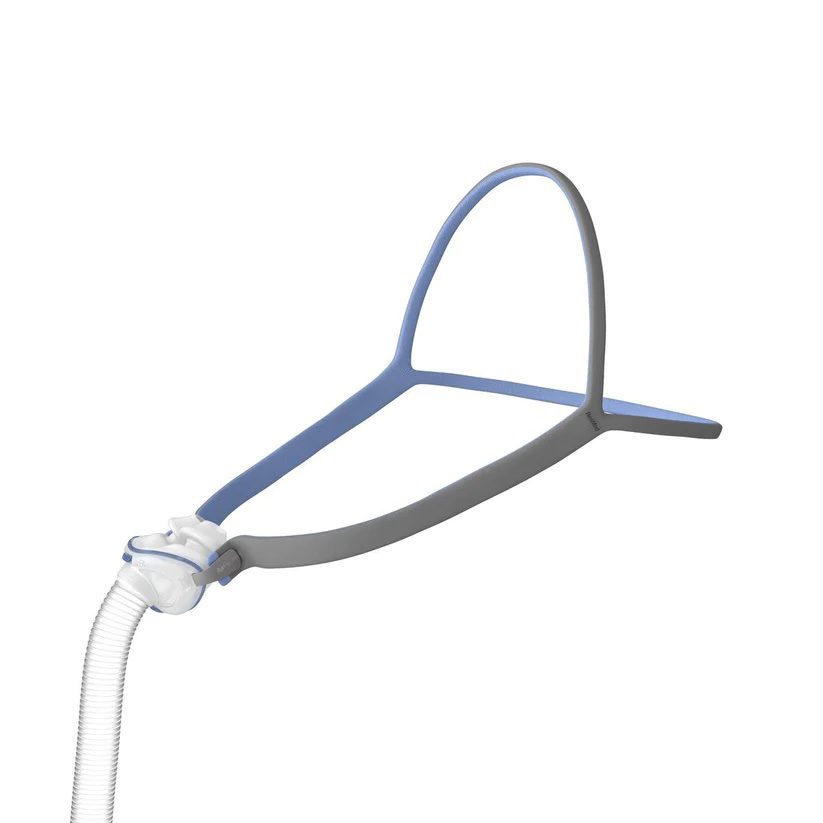
BiPAP machines generate pressurized air that's sent through a hose and delivered to the user’s upper airway via a mask. Most BiPAP masks cover the nostrils, nose, or nose and mouth, though other options are available.
The two air pressure levels used by a BiPAP machine are called inspiratory positive airway pressure (IPAP) and expiratory positive airway pressure (EPAP). The IPAP level, which is generally the higher number of the two, is used during inhalation. The machine switches to EPAP when the user exhales.
The difference in pressure settings between IPAP and EPAP aids inhalation while also making it easier to breathe out against the flow of pressurized air. Most BiPAP machines have additional settings that can be used to help regulate breathing patterns.
BiPAP Modes of Operation
Since BiPAP machines are used for a number of conditions, each with its own treatment requirements, they typically have multiple modes of operation to provide different forms of therapy. If your doctor prescribes BiPAP therapy, they will explain which setting is right for you.
| Spontaneous | A BiPAP machine used in spontaneous mode, or S mode, switches from IPAP to EPAP according to the user’s natural breathing pattern. This mode works well for some people with OSA, though it may be less effective for others, such as those with central sleep apnea. |
| Spontaneous Timed | Spontaneous timed mode, also known as S/T mode, works the same as spontaneous mode unless the machine detects that it has been too long since the user has breathed in. At this point, the machine goes through a programmed IPAP and EPAP cycle to deliver a “backup breath” and facilitate breathing. |
| Timed | Timed mode, or T mode, switches between IPAP and EPAP according to a timed schedule and does not respond to the user’s spontaneous breathing pattern. This setting is used less often than the S or S/T modes, as the difference in timing between ventilation and spontaneous breathing can make breathing more difficult for some people. |
IPAP and EPAP Pressure Settings
After a person has been prescribed a BiPAP machine, they must attend a titration study to determine their correct IPAP and EPAP settings.
The titration, which usually occurs at a sleep clinic, involves the person being fitted with both a mask and electrodes before going to sleep. While they sleep, medical professionals use information gathered from the electrodes as they adjust the IPAP and EPAP settings throughout the night to find optimal levels.
After the titration study, the participant’s doctor is given IPAP and EPAP recommendations based on the air pressure required to control their symptoms during the study.
BiPAP vs. CPAP
BiPAP and CPAP are both forms of positive airway pressure therapy, which uses pressurized air to regulate breathing, but they differ in how they work and when they are usually prescribed.
CPAP machines use a single pressure setting regardless of whether the person is inhaling or exhaling. BiPAP, on the other hand, has two air pressure levels that are set by a clinician and work together to normalize breathing.
What Is a BiPAP Machine Used For?
BiPAP machines are designed to help people who need additional breathing support beyond what standard CPAP therapy provides. They’re commonly used to manage sleep apnea, chronic respiratory diseases, and certain types of heart or lung failure.
Obstructive Sleep Apnea (OSA)
The most common sleep breathing disorder, obstructive sleep apnea is a condition that causes people to experience pauses in breathing during sleep due to an obstruction in their airway. This obstruction is usually caused when muscles and tissues in the throat relax during sleep.
PAP therapy helps treat OSA by using pressurized air to keep the airway open and free of obstructions. Some people with OSA switch from CPAP to BiPAP if they find it difficult to exhale against the CPAP machine’s single pressure level. BiPAP may also be prescribed to people for whom CPAP has been ineffective.
Central Sleep Apnea (CSA)
While people with OSA are trying to breathe past an obstruction, those with central sleep apnea frequently stop making an effort to breathe during sleep.
Some people have CSA without a clear reason, called idiopathic OSA. Others get CSA because of another problem, like Cheyne-Stokes breathing. Conditions like muscular dystrophy or long-term use of strong painkillers can also cause CSA.
There are multiple treatment options for CSA, including PAP therapy using a CPAP, BiPAP, or ASV machine. CPAP is considered the first choice for treating CSA, though BiPAP or ASV may be more effective in some cases.
Chronic Obstructive Pulmonary Disease (COPD)
People with COPD often have trouble exhaling fully, leading to trapped air in the lungs and increased effort to breathe. BiPAP can make breathing easier by reducing pressure during exhalation, allowing for more complete airflow out of the lungs.
Studies have shown that using BiPAP at night can help lower carbon dioxide levels, reduce hospitalizations, and improve quality of life for people with moderate to severe COPD. It’s often prescribed when other treatments, such as supplemental oxygen or medications, don’t fully relieve symptoms.
Heart Failure
BiPAP therapy can be beneficial for people with certain types of heart failure, especially when breathing difficulties occur during sleep. In heart failure, fluid can accumulate in the lungs (a condition called pulmonary congestion), making it harder for the lungs to exchange oxygen and carbon dioxide.
By providing two levels of air pressure—one for inhaling and a lower one for exhaling—BiPAP helps keep the airways open and reduces the work of breathing. This support can improve oxygen levels, lower carbon dioxide buildup, and relieve shortness of breath during sleep.
Hypercapnic Respiratory Failure
Hypercapnic respiratory failure occurs when the body retains too much carbon dioxide due to inadequate ventilation. This can result from conditions that weaken the respiratory muscles or limit lung function, such as severe COPD, neuromuscular disorders, or obesity hypoventilation syndrome.
BiPAP provides additional pressure support during inhalation, which helps move more air into the lungs and promotes more effective carbon dioxide removal. By improving ventilation, BiPAP can stabilize breathing and prevent the dangerous buildup of carbon dioxide in the blood.
Is a BiPAP Machine Right for Me?
While BiPAP is regularly used to treat a number of different conditions, it's often prescribed only after someone has tried CPAP therapy and found it ineffective or too uncomfortable. However, there are some situations when a doctor may prescribe BiPAP therapy before CPAP.
In addition to CPAP and BiPAP, there are other types of PAP machines that use complex algorithms to determine the most appropriate pressure level from breath to breath.
Benefits of BiPAP
BiPAP therapy offers several advantages for people who have trouble tolerating standard CPAP therapy or who need additional breathing support. By delivering two distinct air pressure levels, BiPAP machines can make breathing feel more natural and comfortable, particularly for people with certain medical conditions.
Easier Exhalation and Greater Comfort
Because BiPAP lowers the pressure during exhalation, it can feel less forceful and easier to breathe out compared to CPAP. This feature is especially helpful for people who experience discomfort, bloating, or a sensation of “air trapping” when using continuous pressure. The more natural breathing pattern can lead to better sleep quality and higher therapy adherence.
Improved Ventilation and Oxygen Exchange
BiPAP provides additional support for people who have difficulty moving enough air in and out of the lungs on their own. The higher inspiratory pressure helps deliver more oxygen, while the lower expiratory pressure allows carbon dioxide to be exhaled more effectively. This can help reduce symptoms like morning headaches, fatigue, or confusion that are linked to poor nighttime ventilation.
Side Effects of BiPAP Therapy
All forms of PAP therapy are associated with side effects. While in most cases these side effects are mild, they can make treatment adherence more difficult. Some people find relief from PAP side effects by using therapy accessories.
Dry Mouth, Nose, and Throat
The pressurized air generated by a BiPAP machine can cause the mouth, nose, sinuses, and throat to dry out. This can cause inflammation, soreness, nose bleeds, and sinus congestion that in some cases can impact the effectiveness of BiPAP therapy.
Warm humidifiers and heated tubes can add moisture to the air, making it easier on the throat and nose. Some BiPAP machines have integrated humidifiers, though external humidifiers are also available.
Mask Discomfort
BiPAP masks can be uncomfortable for some people, particularly new users unaccustomed to wearing one each night. Some people experience physical discomfort due to skin irritation or redness, while others find the mask claustrophobic.
Choosing the right mask is the easiest way to prevent mask discomfort, though some people need to try several mask types and models before finding one that works for them. Mask liners, which are made from breathable fabric, can also help prevent irritation or redness.
Depending on your mask type and preferred sleep position, you may find it easier to sleep with a CPAP pillow. These specialized pillows feature cutouts or curves that provide space for a mask and hose.
Other Types of PAP Therapy
| Auto-BiPAP | Automatic BiPAP machines, also called auto-BiPAP, use the clinician’s settings combined with an algorithm to determine the best IPAP and EPAP from breath to breath. Since auto-BiPAP machines use the lowest effective pressure levels for inhalation and exhalation, some people find them more comfortable to use than standard BiPAP machines. Others may find that the changes in air pressure make it more difficult to sleep. |
| APAP | Automatic positive airway pressure (APAP) machines change the air pressure level within a prescribed range depending on the user’s needs. Unlike BiPAP, APAP therapy does not provide two distinct pressure levels for inhalation and exhalation. While some APAP machines have an optional comfort setting called expiratory pressure relief that gently lowers air pressure during exhalation, BiPAP machines allow for a greater difference between inspiratory and expiratory pressure. |
| ASV | Like APAP machines, adaptive servo-ventilation (ASV) machines can adjust air pressure based on a user’s breathing patterns. However, ASV machines are bilevel devices that change air pressure levels according to more sophisticated algorithms, including the ability to force inhalation. Conditions treated with ASV machines include central sleep apnea and Cheyne-Stokes respirations. The latter involves alternating periods of apneic events and hyperventilation. ASV is not recommended for some people with chronic heart failure. |
How Do You Get a BiPAP Machine?
Getting a BiPAP machine requires a prescription from a licensed healthcare provider. Because BiPAP therapy delivers higher and more complex pressure settings than standard CPAP, your doctor will typically order it only after reviewing the results of a sleep study or confirming that CPAP therapy isn’t effective or well tolerated.
Do You Need a Prescription for a BiPAP Machine?
PAP machines, including BiPAP machines, can only be purchased with a prescription from a medical provider.
Purchasing a BiPAP machine from a brick-and-mortar location, whether from a sleep specialist or CPAP retailer, requires customers to either have a physical prescription or a digital prescription sent to the retailer by their doctor. Shoppers can also purchase a BiPAP machine online by uploading or faxing their prescription to the retailer.
Will Insurance Cover a BiPAP Machine?
Health insurance, including Medicaid and Medicare, often covers BiPAP machines and their recurring costs. However, this coverage may only be available under specific circumstances. For example, many providers will only cover the costs of a BiPAP machine for OSA if CPAP therapy has already been attempted and shown to be ineffective.
If you are unsure about whether your provider covers BiPAP therapy, or if you don’t know the circumstances under which it’s covered, it is worth reviewing your provider’s literature or contacting them directly for more information.
Can You Use an FSA or HSA for a BiPAP Machine?
BiPAP machines are considered medical devices and are eligible for purchase using a flexible spending account (FSA), health savings account (HSA), or health reimbursement arrangement (HRA). Most CPAP retailers allow customers to use their FSA or HSA debit card when making a purchase.
Where Can You Buy a BiPAP Machine?
Sleep specialists, brick-and-mortar CPAP retailers, and online CPAP retailers are all common places to buy a BiPAP machine, and each location has its own benefits and drawbacks.
- Sleep specialist: Many sleep specialists stock a small range of BiPAP machines and accessories. While the prices may be higher, buying from your specialist gives you the opportunity to receive in-depth advice based on your unique needs.
- Brick-and-mortar CPAP retailer: With a larger selection and lower prices than most sleep specialists, brick-and-mortar retailers are a convenient choice for many people who want to bring their machine home the same day they purchase it.
- Online CPAP retailer: Online retailers are a good choice for people who are primarily interested in a large selection and low prices. Many online CPAP retailers offer free shipping, and some have a chat feature where customers can ask questions about their products.
Frequently Asked Questions
Many people use a BiPAP machine for years as part of long-term management for sleep apnea or chronic respiratory conditions. The device itself doesn’t limit life expectancy—in fact, regular use can help improve breathing, oxygen levels, and overall health outcomes.
For people with progressive illnesses, such as COPD or neuromuscular disorders, BiPAP therapy can ease symptoms, reduce hospitalizations, and support quality of life for as long as it remains beneficial. Your healthcare provider will periodically reassess your needs and adjust settings or therapy as your condition changes.
The average BiPAP machine costs between $1,700 and $3,000 depending on its manufacturer and features. BiPAP machines are generally more expensive than CPAP machines due to their advanced features and the more complex algorithms involved.
It’s important to choose a BiPAP machine based on how well it meets your needs. If you are unsure which machine is right for you, your doctor or sleep specialist can help guide you toward an appropriate model.
A BiPAP machine is compact—roughly the size of a small shoebox—and designed to sit on a bedside table. It includes a base unit with a built-in motor that generates airflow, a flexible hose that connects to the mask, and often a humidifier chamber to add moisture to the air.
The mask, which can cover the nose, mouth, or both, is held in place with adjustable headgear. Most modern BiPAP machines also feature digital displays, data-tracking capabilities, and quiet operation for comfort and convenience.
Daily, you should wash your mask cushion and tubing with warm water and mild soap, then rinse and let them air-dry completely. Once a week, empty and clean the humidifier chamber, and wipe down the outside of the machine with a damp cloth. Always follow the cleaning instructions in your device’s manual—some parts may be dishwasher-safe or require periodic replacement. Avoid using harsh chemicals, alcohol, or ozone-based cleaners, which can damage components.
Since BiPAP machines are mechanical devices that can help people breathe, they are considered a type of ventilator. The pressurized air generated by a BiPAP machine is delivered through an external mask, making it a noninvasive form of ventilation. More invasive forms of ventilation used for life support involve intubation, in which air is delivered through a tube that’s inserted into the trachea through the nose or mouth.
Still have questions?
Sleep apnea products can be confusing. If you need individualized assistance, post your question to the Sleep Doctor forum.