Air pressure is the most important setting on your CPAP machine. If it’s too low, your therapy won’t be effective, and when it’s too high, you may experience uncomfortable side effects. In the worst-case scenario, these side effects may cause you to stop CPAP therapy altogether.
Fortunately, there are ways to make CPAP therapy more comfortable, even at higher air pressure settings. Understanding how air pressure works and learning some key signs to look for can help you know when you need to ask for a different pressure setting.
Need a CPAP Prescription? Start Here.

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
How CPAP Pressure Settings Are Determined
Obstructive sleep apnea (OSA) occurs when the muscles in your airway relax during sleep, obstructing the flow of air and restricting breathing. CPAP therapy works by blowing pressurized air into your airway and keeping it open. CPAP pressure settings are determined based on observations and measurements of your breathing while you sleep.
Optimal air pressure levels vary depending on factors like the type of mask, your body mass index (BMI), and the anatomy of your airway. Air pressure is measured in centimeters of water, or cm H2O, and most people require a CPAP setting between 4 cm H2O and 20 cm H2O.
In-Lab Titration
When you first start CPAP therapy, your healthcare team will typically perform a titration test, which may be part of the sleep study used to diagnose your sleep apnea or performed on a separate night. You’ll sleep in a sleep lab, wearing a CPAP mask connected to a CPAP machine.
The technician will start the pressure at a lower setting and gradually increase it until they see an acceptable improvement in breathing disruptions. Ideally, CPAP therapy should not only reduce episodes of slowed or stopped breathing (apneas and hypopneas) to fewer than 5 per hour, but also reduce snoring and OSA-related sleep disruption.
APAP Device
APAP machines adjust pressure throughout the night based on your breathing patterns. They’re suitable for people who don’t have any other complicating factors, such as other medical disorders that affect breathing during sleep. It may take up to a couple of weeks to find the right pressure range when using APAP.
A major advantage of APAP is that it enables the machine to deliver a lower average air pressure and raise the pressure only when it’s needed. OSA symptoms can fluctuate throughout the night, depending on your sleep position and sleep stage. With APAP, you can use higher pressure settings when necessary and lower air pressure for the rest of the night.
APAP is also a good option for people whose pressure needs change frequently due to factors like seasonal allergies, medications, or alcohol use before bedtime.
Symptoms of CPAP Pressure Being Too High
It’s common to experience some discomfort when you first start CPAP therapy. It can help to wear the mask and use the machine while you’re awake for short periods, and then increasingly longer periods, to get used to the feel of the air blowing into your mouth or nose.
However, if you continue to experience the following symptoms, your CPAP pressure may be too high:
- Dry mouth or nose
- Trouble exhaling
- Feeling like you’re suffocating
- Chest or sinus discomfort
- Bloating, belching, or flatulence from swallowing too much air (aerophagia)
Side Effects of CPAP Pressure Being Too High
Continuing to use a CPAP device with excessively high air pressure settings can have negative consequences for your CPAP therapy.
- Mask leaks: Too-high pressure can cause air to escape from your mask, which not only contributes to a dry mouth and eyes but can also, paradoxically, lead to a drop in the air pressure you receive.
- Reduced compliance: High air pressure can be uncomfortable, and it may make you less likely to use CPAP therapy.
- Reliance on the ramp feature: The ramp function briefly lowers the air pressure and is designed to be used once per night, as you’re falling asleep. Using it repeatedly to avoid uncomfortably high air pressure may mean you receive little to no CPAP air for large portions of the night.
- Development of treatment-emergent central sleep apnea: Unlike obstructive sleep apnea, which is caused by a physical obstruction, central sleep apnea occurs when the brain fails to send the signal to breathe. A small number of people who use high-pressure CPAP settings may develop symptoms of central sleep apnea.
What to Do if Your CPAP Pressure Is Too High
Talk to your doctor if you believe your CPAP air pressure may be too high. It’s important not to change the settings yourself, as this may affect your therapy.
In some cases, high CPAP air pressure may be uncomfortable but necessary. If you require high air pressure to address your sleep apnea, there are several features designed to make these strong settings more tolerable.
- Ramp: The ramp setting starts your CPAP machine at a lower level and gradually increases the pressure over a period of approximately 5 to 45 minutes to let you fall asleep more easily.
- Pressure Relief: Expiratory pressure relief (EPR) delivers slightly gentler airflow when you are breathing out, as some people find it counterintuitive to exhale against air coming in.
- APAP: APAP is increasingly common on modern PAP machines and is a good option if you have trouble tolerating high air pressures. Your doctor can choose a pressure range within which the machine can fluctuate throughout the night.
- BiPAP: If you require pressure settings over 15 cm H2O, your doctor may prescribe bi-level positive airway pressure (BiPAP), which delivers your normal pressure when breathing in and a significantly lower pressure when breathing out. You’ll need to redo an in-lab titration study before switching to BiPAP.
Sometimes your CPAP side effects may require some troubleshooting beyond the pressure level. For example, symptoms due to the cold, dry air can be solved by using a heated humidifier. For nasal congestion, doctors may give you a nasal spray or antihistamines.
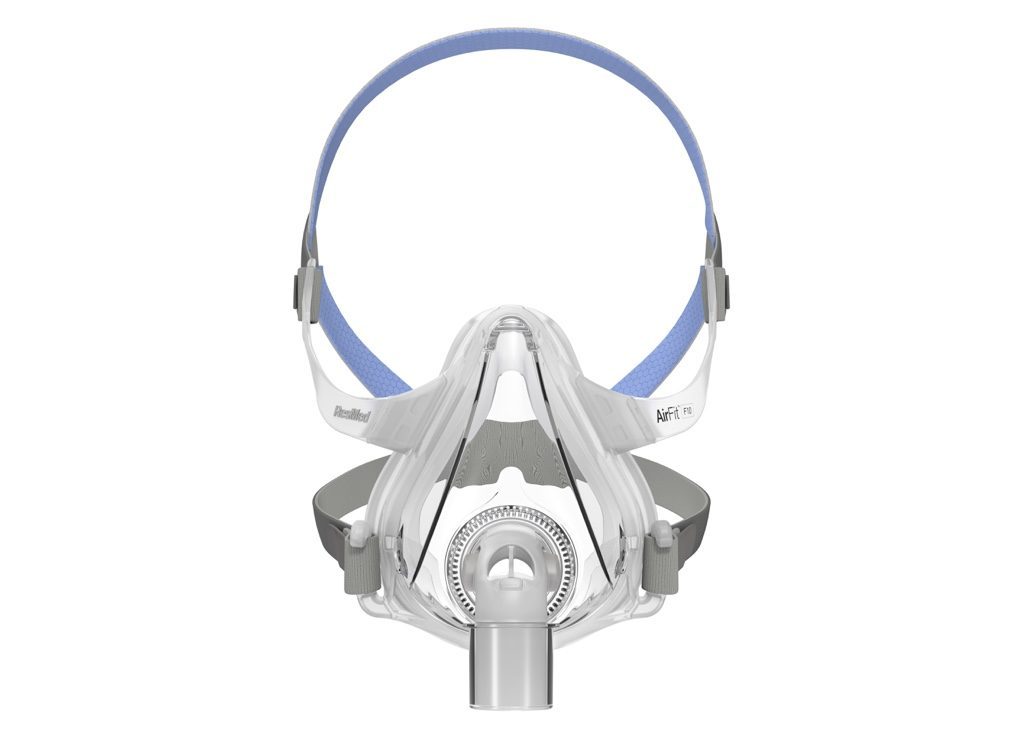
Changing the type of mask may also help therapy feel more comfortable or allow you to use lower air pressure settings. Since nasal pillows masks blow air directly into the nostrils, they’re not usually used by people who have pressure settings over 12 cm H2O. Studies suggest that nasal masks may require lower pressure settings than full-face masks, but full-face masks may feel subjectively gentler.
If your sleep apnea symptoms tend to be worse when lying on your back, you may be able to get away with a lower fixed pressure setting if you find a way to avoid back sleeping, such as sewing a tennis ball into the back of your shirt.
Since CPAP therapy is quite personal, you and your doctor can experiment together to find a system that works for you without sacrificing the quality of your therapy.
When to Talk to Your Doctor
It’s normal to take some time to adjust to CPAP therapy when you first start using it. Experts recommend scheduling a follow-up visit with your provider a few weeks after starting CPAP therapy, so you can work through any issues together. If they think it’s necessary, your sleep specialist may perform another titration study to confirm if your air pressure settings are correctly calibrated.
Studies suggest that it’s common for people to be assigned a CPAP pressure setting that’s not optimal, so don’t be afraid to voice your concerns to your doctor if you suspect your pressure settings are too high or too low.
You may also want to talk to your doctor if you’ve been using CPAP therapy for a while and you start experiencing new side effects or the return of sleep apnea symptoms. Before scheduling a visit, you can get an idea of how well your therapy is working by reading the data provided by your CPAP device. Most modern CPAP devices track key metrics like the number of breathing events you experience during sleep and whether you’ve had any air leaks.
Gaining or losing a lot of weight, experiencing changes to your teeth or bite, or switching to a different CPAP mask model can all affect the pressure requirements from your CPAP machine. If any of these situations apply to you, you should request that your doctor reassess your pressure settings.
Frequently Asked Questions
There’s no specific pressure at which CPAP therapy works best for everyone, although most people end up using a pressure setting between 4 cm H2O and 20 cm H2O. Your doctor will establish the minimum pressure needed for your individual treatment based on your sleep test and titration study. Alternatively, you can use an APAP device that changes the pressure automatically throughout the night as needed.
Yes, reducing your CPAP pressure below the minimum amount needed to keep your airway open can make therapy less effective and lead to the return of your sleep apnea symptoms.
While you can make slight adjustments using the ramp feature or expiratory pressure relief, you shouldn’t touch the actual pressure settings by yourself. Instead, talk to your doctor if you find the air pressure too strong or too weak.
Your CPAP mask may leak air if it doesn’t fit properly, if the headgear is over-tightened, if the materials are getting old and stiff, or if your therapy pressure is set too high. You may also experience CPAP air escaping through the mouth — called a “mouth leak” — if you breathe through your mouth while using a nasal mask. This can cause a dry mouth, but it’s easily fixed by using a chin strap or switching to a full-face mask.