Using a CPAP machine can significantly improve your sleep apnea, but if you’re breathing through your mouth during the night, you might not be getting the full benefits. Mouth breathing during sleep causes changes in the airway that may worsen obstructive sleep apnea (OSA). It can also lead to dry mouth, sore throat, air leaks, and even reduced therapy effectiveness.
Whether you're new to CPAP or trying to fine-tune your setup, preventing mouth breathing is an important step toward more comfortable—and more effective—sleep apnea treatment.
How to Know if You’re a CPAP Mouth Breather
First of all, you might not even realize you're breathing through your mouth while on a CPAP machine. However, there are a few signs that can suggest this is the case.
- Waking up with a dry mouth, sore throat, or nasal congestion
- Your partner notices you snoring, even with your CPAP on
- Often waking up feeling tired or unrested
- Breathing through your mouth when you fall asleep or during the day
How to Keep Your Mouth Shut With CPAP
Keeping your mouth closed during CPAP therapy is key to getting the full benefits of your treatment. When your mouth stays shut, the pressurized air stays in your airway—helping prevent snoring, leaks, and disrupted sleep.
If you’re a mouth breather, don’t worry—there are several simple strategies that can help you train your body to breathe through your nose and stay more comfortable through the night.
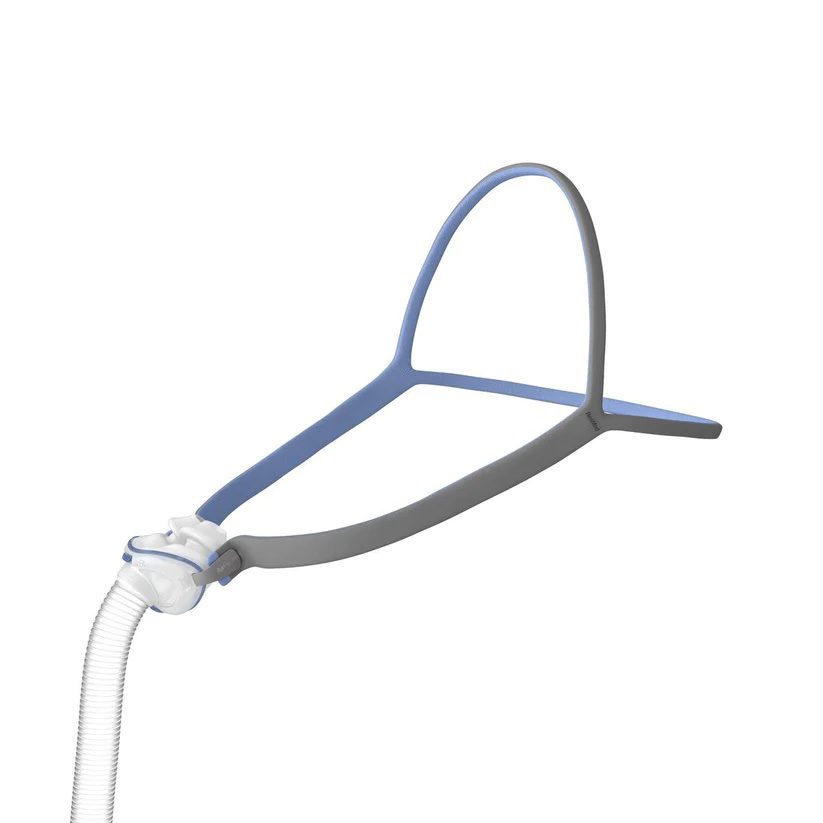
Consider a Chin Strap
To prevent unintended air leaks during CPAP treatment, your doctor may recommend a chin strap that keeps your mouth closed during sleep. This helps ensure that the air delivered through the CPAP mask reaches the airway and is not lost through the mouth. Chin straps are available in various designs, but their purpose is to gently prevent mouth breathing.
Try Mouth Taping
Some health care providers may also suggest mouth taping. While chin straps can prevent the jaw from opening, they may not always prevent air from escaping the lips. There are various products that have been developed for mouth taping. Talk to your doctor for more information.
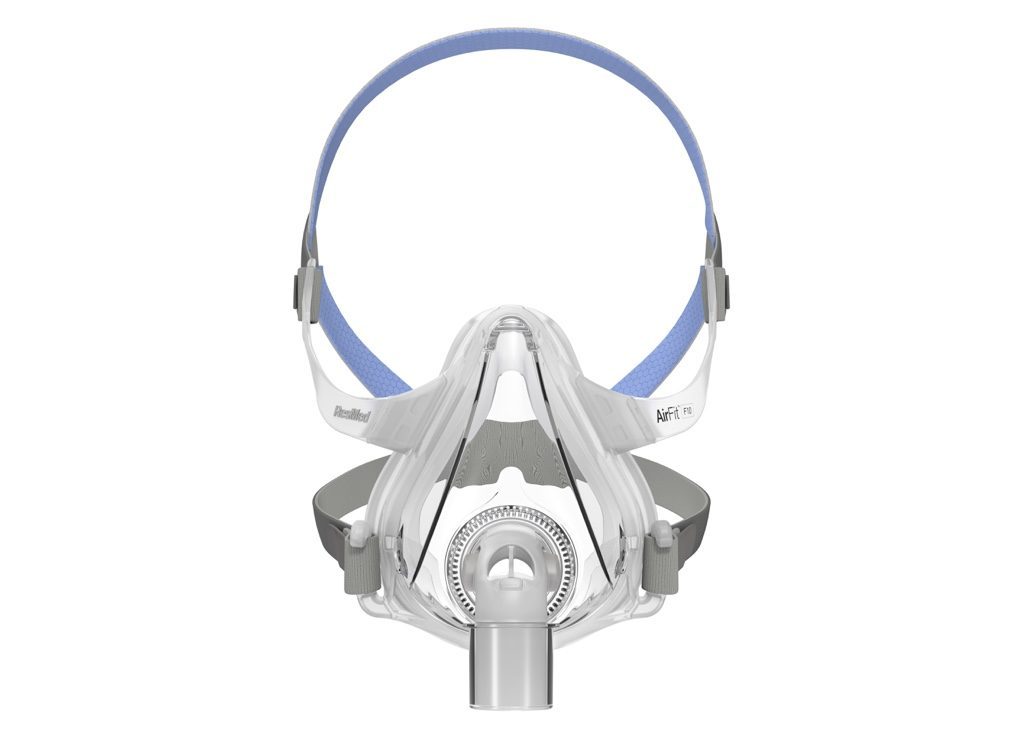
Switch to an Oronasal Mask
If a chin strap doesn’t stop air from leaking through your mouth while you sleep, your doctor may recommend changing the type of mask you use for CPAP therapy. Unlike nasal masks or nasal pillows that deliver pressurized air only through the nose, an oronasal mask sends air through both the nose and the mouth.
Keep Your Sinuses Clear
When your nose is blocked due to congestion or other causes, you may breathe through your mouth instead. Keeping your sinuses clear can help reduce mouth breathing and make it easier to use your CPAP consistently.
One approach to reducing nasal congestion is to use a CPAP humidifier to add moisture to the air and soothe dry nasal passages. To ensure you receive the right level of moisture during sleep, fill the reservoir to capacity before bedtime and allow it to empty almost completely by morning.
Another option is prescription nasal steroids to reduce inflammation and congestion in the nasal passages. If structural issues in the nose are contributing to symptoms, a doctor may recommend nasal or sinus surgery.
Practice Nasal Breathing During the Day
Training yourself to breathe through your nose during the day can make it easier to do the same at night while using CPAP. Start by being mindful of your breathing patterns—whether you’re working, walking, or relaxing, make a conscious effort to keep your mouth closed and breathe through your nose. Over time, this practice can help retrain your body’s default breathing habits, reduce mouth breathing during sleep, and improve the effectiveness of your CPAP therapy.
Causes of Mouth Breathing on CPAP
People who are prescribed CPAP therapy often have obstructive sleep apnea (OSA), a condition linked to mouth breathing. Most people breathe through their nose during sleep. However, people with OSA tend to breathe through their nose and their mouth. Other common causes of mouth breathing on CPAP include:
- Nasal congestion: Allergies, colds, or a deviated septum can make nose breathing difficult.
- Habitual mouth breathing: Long-standing daytime habits can carry over into sleep.
- Jaw relaxation during sleep: Muscles naturally relax during deeper sleep, causing the mouth to fall open.
- Dry airflow: Air that’s too dry can irritate the nasal passages, leading to mouth breathing for relief.
Additionally, mouth breathing becomes more common as people get older. Other risk factors for mouth breathing in people with OSA include:
- Obstructions in the nose
- More severe OSA
- A larger neck
- Obesity
- Being born male
Potential Risks of CPAP Mouth Breathing
In addition to potential side effects like dry mouth and nasal congestion, mouth breathing can also decrease the effectiveness of treatment and make it more difficult to use CPAP as recommended.
In order to get the full benefits of CPAP therapy, it’s important to use the machine consistently through the night. Research has found that people who use nasal masks and breathe through their mouths during sleep are less likely to use their machines as often as recommended.
Additionally, early research suggests that people with OSA may be at a heightened risk of developing gum disease. One potential explanation of this association is that mouth breathing and dry mouth can contribute to a buildup of bacteria and plaque in the mouth.
When to Talk to Your Doctor
If your CPAP therapy makes you uncomfortable or causes other problems, talk to your doctor. Doctors can help find the cause of side effects, discuss solutions, and help you get the most out of CPAP therapy.