At a Glance
Medicare covers CPAP machines when they’re prescribed to treat obstructive sleep apnea and medical necessity requirements are met. Coverage is provided under Medicare Part B, typically through a rental period before ownership, though you’ll be responsible for any applicable copays.
CPAP therapy is one of the most effective treatments for sleep apnea, but the cost can raise questions about insurance coverage. Medicare covers CPAP machines and related supplies when certain medical and usage requirements are met. This guide explains coverage, eligibility, compliance rules, and expected costs.
Need a CPAP Prescription? Start Here

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
Medicare CPAP Coverage
If you’ve been diagnosed with sleep apnea and prescribed CPAP therapy, you can get Medicare coverage by following specific steps. Medicare considers CPAP machines and accessories durable medical equipment (DME) that’s medically necessary when a physician prescribes them for sleep apnea treatment. DME, including CPAP machines and accessories, is covered under Medicare Part B, the section of Medicare that covers supplies, preventative care, and outpatient services.
However, instead of covering the cost of the machine outright, Medicare covers a trial period and a CPAP machine rental.
Who’s Eligible?
You qualify for Medicare CPAP coverage if a physician diagnoses sleep apnea on a qualifying in-lab or home sleep study. Medicare may also help cover the cost of sleep studies needed to diagnose sleep apnea and other specific sleep disorders.
What’s Covered?
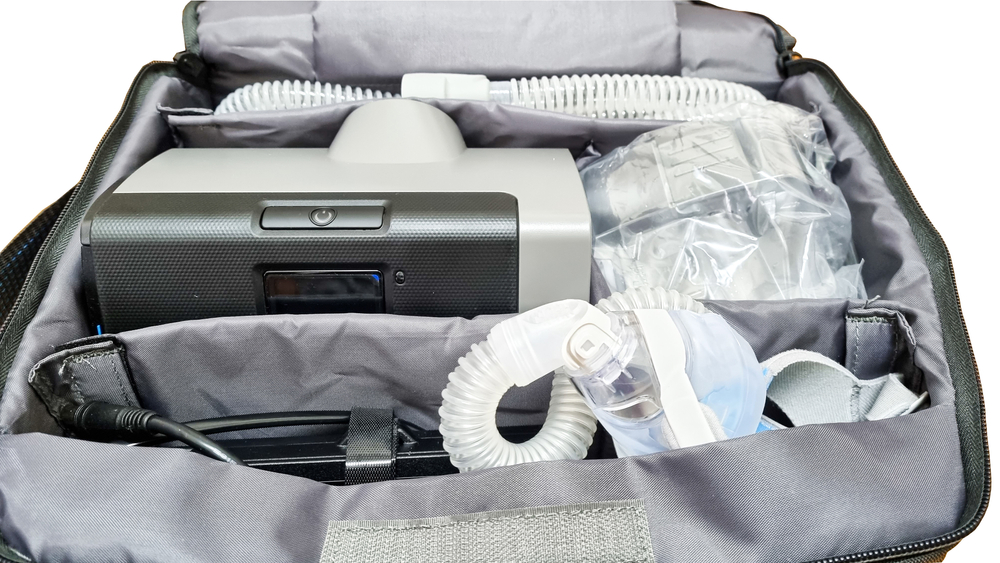
Once a doctor prescribes CPAP therapy, Medicare may cover a 12-week trial. The trial includes the device and necessary accessories. During the 12-week trial, you will meet with your physician to see if CPAP therapy is helping and you are compliant with therapy. Medicare will then continue to cover a 13-month CPAP machine rental and then pay off the device for you to own at the end of this period.
After you meet your Part B deductible, Medicare covers 80% of Medicare-approved costs, and you’ll be responsible for the remaining 20%. Part B covers medically necessary CPAP DME during the trial and rental periods. That includes a CPAP machine, humidifier, mask, cushion, tubing, headgear, and other specific accessories. It also covers regular device and component replacements.
Medicare requires ongoing documentation showing both clinical benefit and consistent use. This usually is evaluated during a yearly visit with your physician to renew CPAP and CPAP supply coverage.
How Do You Qualify?
To buy a CPAP machine out of pocket or through Medicare, you need a prescription. In order to qualify for coverage, your CPAP machine and accessories must be considered medically necessary by Medicare.
First, a physician needs to diagnose you with sleep apnea after reviewing the data from an in-person or at-home sleep study. Once you’ve been prescribed CPAP therapy, you can qualify for Medicare coverage. Without documented sleep study results and a valid prescription, Medicare will not cover CPAP equipment.
Medicare and CPAP Compliance
During the 12-week trial period and 13-month rental, Medicare will only cover your CPAP costs if you adhere to therapy. Most CPAP machines record sleep data that your physician and Medicare can review. Most newer CPAP models transmit usage data automatically.
Medicare requires that you use the machine for at least 4 hours per night over a consecutive 30-day period within the first 90 days of trying CPAP. You must meet this threshold on 70% of nights.
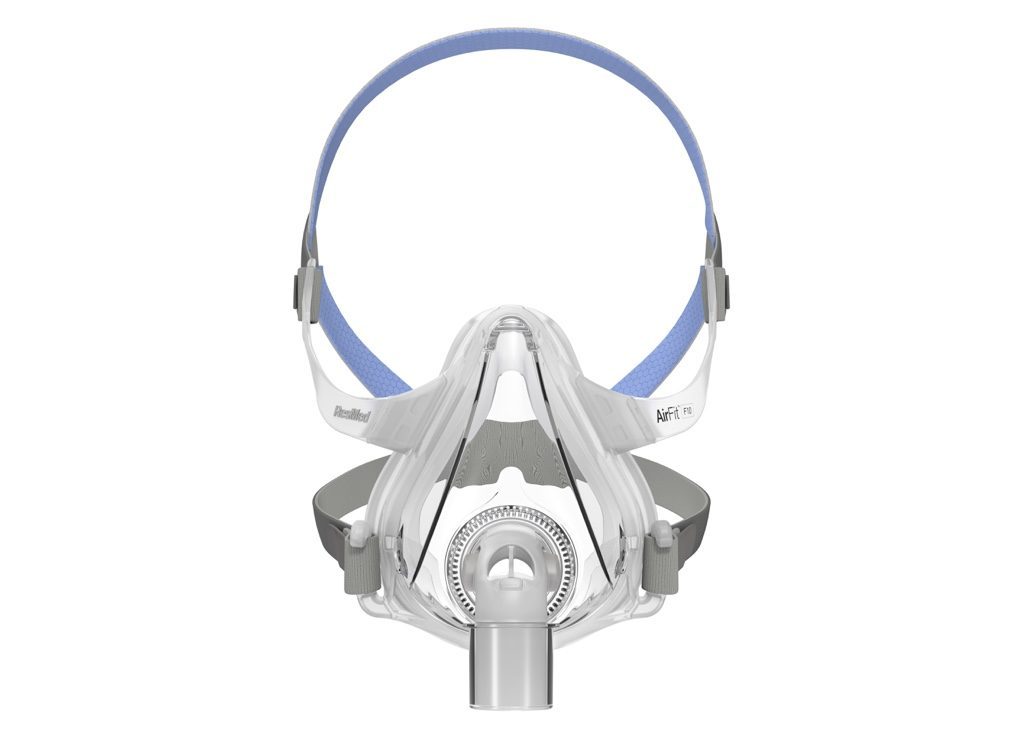
Poor mask fit and discomfort remain the top reasons for noncompliance. Mask refitting, pressure adjustments and humidification improve comfort and adherence.
Does Medicare Cover CPAP Supplies?
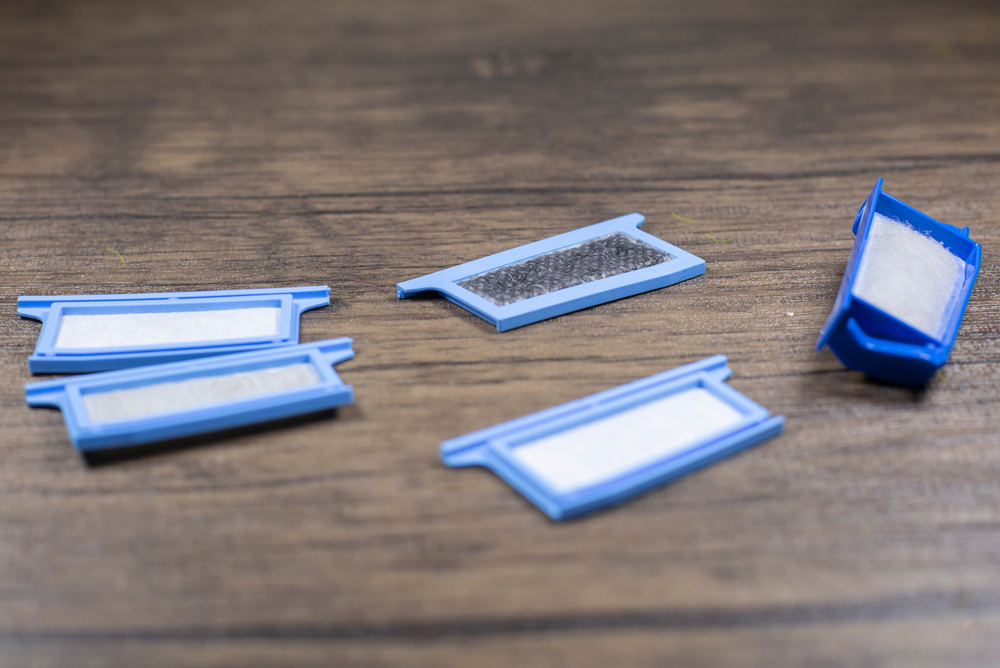
After you meet your deductible, Medicare Part B covers 80% of DME costs. That means you’ll only pay 20% of the cost of a CPAP supplies including a humidifier, tubing, hose, mask, cushion, filters, and headgear. Accessories like mask liners and CPAP cleaners aren’t covered.
Medicare CPAP Supplies Replacement Schedule
Medicare covers CPAP supply and accessory replacements on a regular schedule.
| Item | Replacement Frequency |
|---|---|
| Full-face masks | Every three months |
| Nasal pillows and cushions | Monthly |
| Oralnasal mask cushions | Monthly |
| Mask frames | Every 3 months |
| Mask headgear | Every 6 months |
| Disposable air filters | Monthly |
| Hoses and tubing | Every 3 months |
| Humidifier chamber | Every 6 months |
| CPAP or BiPAP machine | Every 5 years |
Frequently Asked Questions
Medicare covers several treatments for sleep apnea. The most common and widely used is CPAP therapy. Medicare Part D also covers Zepbound for sleep apnea for people with an OSA diagnosis and a BMI of 27 or higher. A mandibular advancement device or oral appliance for treatment of sleep apnea can also be covered. Inspire sleep apnea treatment may also be covered for people who meet specific criteria.
Medicare covers 80% of a CPAP machine cost after you meet your Part B deductible, so you’ll pay for your deductible plus 20% of the device’s cost. However, you won’t own the CPAP machine outright until you use it correctly and regularly for 13 months. During those 13 months, the CPAP machine is a rental.
CPAP machine costs can vary, but they’re most often between $800 and $1,200. After meeting your deductible, you’ll be responsible for 20% of the cost. Budget for an out-of-pocket cost between $150 and $250, plus your deductible.
Generally, Medicare covers a new CPAP, APAP, or BiPAP machine every 5 years. If a machine is recalled or breaks, you may be able to get a new one sooner. Normal wear alone does not qualify for early replacement.