There are two types of positive airway pressure systems often used to treat sleep apnea, continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP or BPAP). Both work via machines that help direct air into the airway and lungs.
While CPAP and BiPAP are similar, they do have some differences in how they work. Thus, doctors may recommend one type of machine over another, depending on your situation. We discuss CPAP and BiPAP therapies, their features, indications, and situations where they may be best utilized.
What’s the Difference Between CPAP and BiPAP?
CPAP and BiPAP machines are both positive airway pressure treatments for sleep apnea, but they differ in how they work, how much they cost, and whether they are covered by insurance.
Both types of positive airway pressure (PAP) therapy push air into the upper airway and lungs through the nose or the nose and mouth using a machine. The pressurized air prevents the airway from narrowing or collapsing during sleep.
| CPAP | BPAP | |
|---|---|---|
| Range of Pressure | 4-20 cm H20 | 4-30 cm H20 |
| Pressure Level | 1 | 2 |
| Cost | $500 – $1,000 | $1,700 – $3,000 |
| Insurance Coverage | Yes, though costs vary depending on the plan | Depends on the circumstances |
Pressure
The level of air pressure during inhalation and exhalation varies depending on the type of PAP therapy a person is prescribed.
CPAP machines deliver the same pressure when breathing in and breathing out. In contrast, BiPAP machines provide two different pressure levels, one level of air pressure during inhalation and a lower level for exhalation.
Cost and Insurance Coverage
The cost and insurance coverage for CPAP and BiPAP therapies vary. CPAP machines cost anywhere from $500 to $1,000. BiPAP machines are typically more expensive than a CPAP machine, with a price range of $1,700 to $3,000.
CPAP therapy is often covered by private health insurance. It’s important to check with your insurance provider because coverage varies depending on your insurance policy. In addition, it’s important to talk with your insurance company about coverage for CPAP supplies, such as masks and replacement filters, so you understand the full cost of therapy.
If you use Medicare and require CPAP therapy, you may be provided a three-month trial of CPAP therapy that includes a CPAP machine and accessories. After you meet with your doctor and they review data from your trial period, Medicare may continue coverage for your CPAP therapy.
BiPAP may only be covered by your insurance company or Medicare if you meet certain criteria. For example, BiPAP therapy may not be covered unless you are intolerant of CPAP therapy or CPAP is ineffective at treating your sleep apnea.
Recommended Use for CPAP and BiPAP
The recommendations for who should use CPAP and who should use BiPAP depends on the type of sleep apnea a person has and whether they have responded to other types of treatments.
CPAP therapy is the treatment of choice for most people with obstructive sleep apnea. If used properly, CPAP effectively treats most cases of OSA.
In contrast, BiPAP machines are the preferred treatment for people who have complex sleep-related breathing issues, including severe OSA that requires very high pressure levels. It may also be recommended for people with sleep-related hypoxemia, where the blood oxygen levels are too low, or sleep-related hypoventilation, where the blood carbon dioxide levels are too high.
Understanding CPAP Machines
CPAP machines work by delivering a continuous pressure of air as a person breathes in and out. This means that the air pressures for inhalation and exhalation are set at the same level.
Many CPAP devices deliver the same pressure levels throughout the night. This is known as fixed-level CPAP. Alternatively, auto-adjusting CPAP (APAP) machines allow air pressure to vary throughout the night depending on a person’s breathing patterns. Some people may tolerate APAP better because the average overnight pressure tends to be lower than for fixed CPAP.
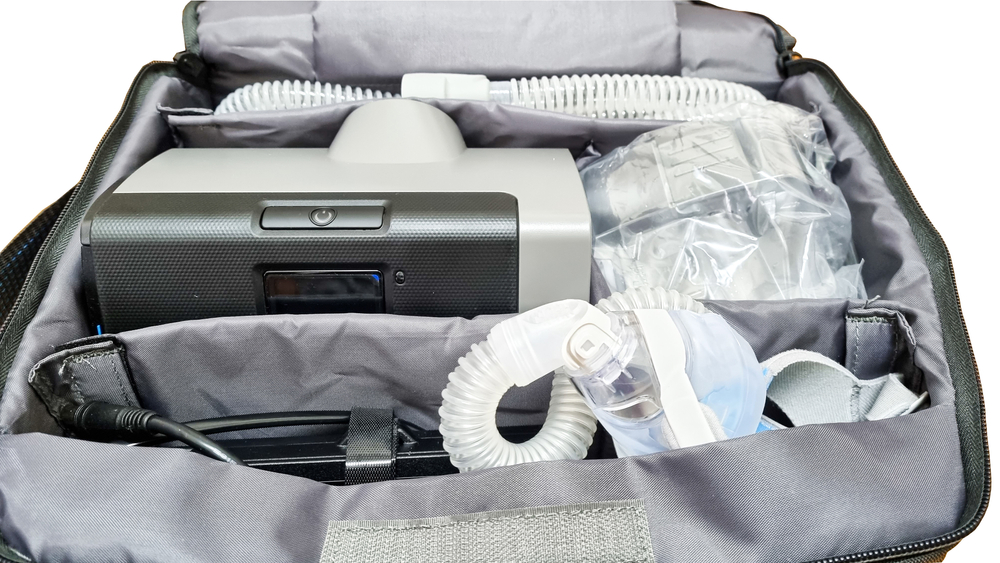
All CPAP machines usually come standard with the following:
- A machine that blows air into a tube or hose
- A tube or hose that connects the machine to the face mask
Newer CPAP machines may also come with additional features such as heated humidifiers that blow warm, moist air into the airway to reduce nasal dryness.
When Is CPAP Prescribed?
Experts, including the American Academy of Sleep Medicine (AASM), recommend CPAP for obstructive sleep apnea (OSA). The air pressure from the machine works to keep blocked airways open, which reduces snoring, improves sleep quality, and improves daytime symptoms. In some cases, CPAP is also used to treat central sleep apnea.
Doctors may try fixed-level CPAP or auto-adjusting CPAP (APAP) for people with sleep apnea. The pressure settings that work best for an individual are based upon sleep study results. Experts recommend fixed-level CPAP instead of APAP for those with OSA and other conditions such as:
- Severe chronic obstructive pulmonary disease
- Congestive heart failure
- Medication or drug-related breathing complications
- Central sleep apnea
- A history of having certain upper airway surgeries
- People who may have a mask leak due to certain facial characteristics
Auto-adjusting CPAP may be an option for people with moderate or severe OSA that is not complicated by other health concerns that affect the ability to breathe during sleep. APAP may also be an option for people with mild OSA or those who cannot tolerate fixed-level CPAP.
Understanding BiPAP Machines
Unlike CPAP that delivers a steady air pressure as a person inhales and exhales during sleep, BiPAP delivers air at different pressure levels, one for inhalation and one for exhalation. The pressure setting for inhalation (inspiratory positive airway pressure or IPAP) is higher than the pressure setting for exhalation (expiratory positive airway pressure or EPAP).
BiPAP machines usually come with a similar set of equipment as CPAP machines, including a motorized machine, tubing, a mask, and other special features.
Like CPAP devices, BiPAP machines can be either fixed or auto-adjusting.
- Fixed-level BiPAP: With a fixed-level BiPAP machine, pre-determined IPAP and EPAP settings are programmed into the machine and do not change at any point throughout sleep.
- Auto-adjusting BiPAP: Auto-adjusting BiPAP, or auto-BiPAP, machines automatically deliver varying EPAP and IPAP levels to accommodate different breathing patterns. This is ideal for people who are not able to tolerate the pre-set, fixed pressures that are delivered while asleep.
BiPAP machines also have several unique modes.
- Spontaneous (S): In spontaneous mode, the machine is triggered when a person breathes in or out. BiPAP-S mode may be used for people with OSA who do not respond to CPAP, those who find CPAP to be uncomfortable, or people with OSA and conditions that cause hypoventilation.
- Spontaneous/timed (S/T): The machine has a timer and will deliver a breathing cycle if a person has not taken a breath for a period of time. This setting is known as a backup rate and is typically used for people with CSA or for people whose breathing is too weak to trigger the BiPAP machine’s cycle.
- Timed (T): In this mode, the BiPAP machine delivers breathing cycles only according to a timer and not in response to a person’s breathing. BiPAP-T mode is rarely used because S/T provides the same functionality.
When Is BiPAP Prescribed?
BiPAP S/T is proven to effectively treat some types of central sleep apnea and can be an alternative for people who have had difficulty with CPAP therapy.
Certain BiPAP modalities are the recommended treatment for people who have a combination of obstructive and central sleep apnea. It is also the treatment of choice for central sleep apneas that are related to certain health conditions that can cause shallow or slow breathing during sleep including:
- Central nervous system disease, such as multiple sclerosis
- Neuromuscular disease, such as muscular dystrophy
- Opioid use
- Chronic obstructive pulmonary disorder (COPD)
While CPAP therapy effectively treats obstructive sleep apnea in most people, some people may benefit from using BiPAP instead. Sleepers that require an air pressure that exceeds the pressure range available on a CPAP machine may be prescribed BiPAP as an alternative.
In some instances, people prescribed CPAP therapy struggle with treatment and are unable to continue. In other cases, CPAP therapy does not adequately treat sleep apnea. In both situations, BiPAP can be an effective alternative to CPAP.
BiPAP vs. CPAP: Which Is Best for You?
The type of PAP machine that is best for you depends on the type of sleep apnea you are diagnosed with as well as your response to other sleep apnea treatments. Your doctor or sleep specialist will talk with you about the available options and what type of PAP therapy is best for your situation.
In general, experts agree that CPAP therapy is the best treatment for obstructive sleep apnea that is not complicated by other health issues that affect breathing during sleep.
The best treatment for people with more complex sleep-related breathing issues, such as those with certain types of central sleep apnea, is often BiPAP. BiPAP therapy can also be a helpful option for people who cannot tolerate CPAP therapy or whose OSA does not respond to CPAP treatment.