There are two types of positive airway pressure systems often used to treat sleep apnea, continuous positive airway pressure (CPAP) and bilevel positive airway pressure (BiPAP or BPAP). Both work via machines that help direct air into the airway and lungs.
While CPAP and BiPAP are similar, they do have some differences in how they work. Thus, doctors may recommend one type of machine over another, depending on your situation. Below, we discuss CPAP and BiPAP therapies, their features, indications, and situations where they may be best utilized.
Need a CPAP Prescription? Start Here.

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
What’s the Difference Between CPAP and BiPAP?
CPAP and BiPAP machines are both positive airway pressure treatments for sleep apnea, but they differ in how they work, how much they cost, and whether they're covered by insurance.
Both types of positive airway pressure (PAP) therapy push air into the upper airway and lungs through the nose or the nose and mouth using a machine. The pressurized air prevents the airway from narrowing or collapsing during sleep.
Pressure
The level of air pressure during your inhale and exhale varies depending on the type of PAP therapy a person is prescribed.
- CPAP machines deliver the same pressure when breathing in and breathing out.
- BiPAP machines provide two different pressure levels, one level of air pressure during inhalation and a lower level for exhalation.
Cost and Insurance Coverage
The cost and insurance coverage for CPAP and BiPAP therapies vary. CPAP machines cost anywhere from $500 to $1,000. BiPAP devices are typically more expensive than a CPAP machine, with a price range of $1,700 to $3,000.
CPAP therapy is often covered by private health insurance, but it’s important to check with your insurance provider because coverage varies depending on your policy. In addition, it’s important to talk with your insurance company about coverage for CPAP supplies, such as masks and replacement filters, so you understand the full cost of therapy.
If you use Medicare and require CPAP therapy, you may be provided a three-month trial of CPAP therapy that includes a CPAP machine and accessories. After you meet with your doctor and they review data from your trial period, Medicare may continue coverage for your CPAP therapy.
BiPAP may only be covered by your insurance company or Medicare if you meet certain criteria. For example, BiPAP therapy may not be covered unless you are intolerant of CPAP therapy or CPAP is ineffective at treating your sleep apnea.
Recommended Use for CPAP and BiPAP
The recommendations for who should use CPAP and who should use BiPAP depends on the type of sleep apnea a person has and whether they have responded to other types of treatments.
CPAP therapy is the treatment of choice for most people with obstructive sleep apnea. If used properly, CPAP effectively treats most cases of OSA.
In contrast, BiPAP machines are the preferred treatment for people who have complex sleep-related breathing issues, including severe OSA that requires very high pressure levels. It may also be recommended for people with sleep-related hypoxemia, where the blood oxygen levels are too low, or sleep-related hypoventilation, where the blood carbon dioxide levels are too high.
| CPAP | BPAP | |
|---|---|---|
| Range of Pressure | 4-20 cm H20 | 4-30 cm H20 |
| Pressure Level(s) | 1 | 2 |
| Cost | $500 – $1,000 | $1,700 – $3,000 |
| Insurance Coverage | Yes, though costs vary depending on the plan | Depends on the circumstances |
What Is CPAP?
CPAP machines work by delivering a continuous pressure of air as a person breathes in and out. This means that the air pressures for inhalation and exhalation are set at the same level. Many CPAP devices deliver the same pressure levels throughout the night. This is known as fixed-level CPAP.
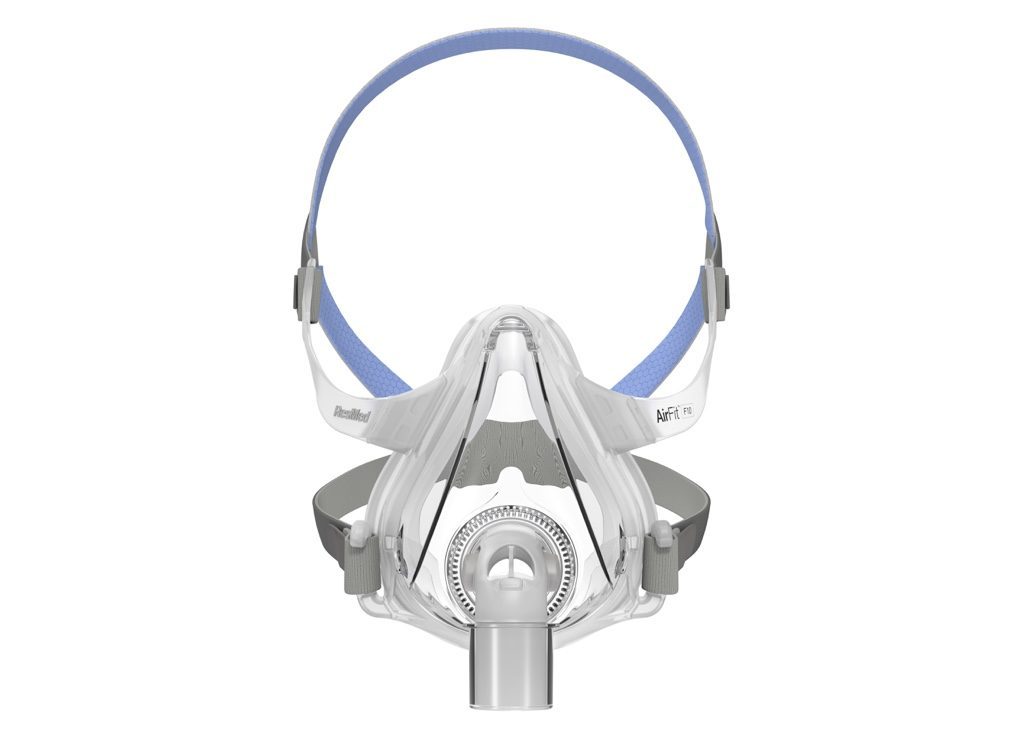
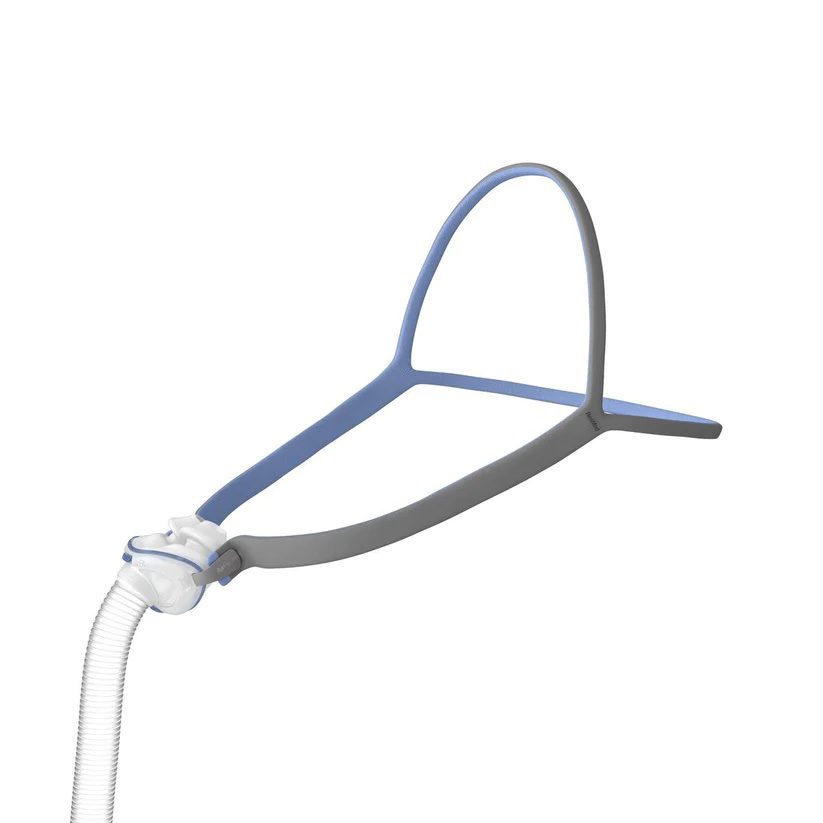
All CPAP machines usually come standard with the following:
- A machine that blows air into a tube or hose
- A tube or hose that connects the machine to the face mask
Newer CPAP machines may also come with additional features such as heated humidifiers that blow warm, moist air into the airway to reduce nasal dryness.
What Are the Benefits of CPAP?
While both CPAP and BiPAP are effective treatments for sleep apnea, CPAP is often the first-line therapy. For many users, CPAP offers a simpler, more accessible approach to therapy. The benefits of CPAP over BiPAP include:
- Simplicity: CPAP machines are easier to operate, with fewer settings to adjust.
- Lower cost: CPAP devices tend to be more affordable than BiPAP machines, both upfront and over time.
- Wider availability: CPAP is more commonly prescribed and more readily available through sleep clinics and insurance providers.
- Effective for most cases: CPAP is usually sufficient for treating mild to moderate obstructive sleep apnea without the need for pressure variation.
What Are the Drawbacks of CPAP?
Although CPAP therapy is effective for many people with OSA, it’s not ideal for everyone. Some potential drawbacks of CPAP compared to BiPAP include:
- Less comfortable exhalation: The fixed pressure can make it harder for some people to breathe out naturally.
- Limited pressure flexibility: CPAP machines don’t automatically adjust between breaths, which may be less suitable for people with higher pressure needs or coexisting respiratory conditions.
- Not ideal for central sleep apnea: CPAP may be less effective for people with central or complex sleep apnea, where the issue isn’t just a blocked airway but a lack of breathing effort.
Who Is CPAP Best For?
Experts, including the American Academy of Sleep Medicine (AASM), recommend CPAP for obstructive sleep apnea (OSA). The air pressure from the machine works to keep blocked airways open, which reduces snoring, improves sleep quality, and improves daytime symptoms. The pressure settings that work best for an individual are based upon sleep study results.
In general, doctors recommend CPAP for those with conditions such as:
- Obstructive sleep apnea (OSA)
- Severe chronic obstructive pulmonary disease (COPD)
- Congestive heart failure
- Medication or drug-related breathing complications
- A history of having certain upper airway surgeries
- People who may have a mask leak due to certain facial characteristics
What Is BiPAP?
Unlike CPAP that delivers a steady air pressure as a person inhales and exhales during sleep, BiPAP delivers air at different pressure levels, one for inhalation and one for exhalation. The pressure setting for inhalation (inspiratory positive airway pressure or IPAP) is higher than the pressure setting for exhalation (expiratory positive airway pressure or EPAP).
BiPAP machines usually come with a similar set of equipment as CPAP machines, including a motorized machine, tubing, a mask, and other special features.
Like CPAP devices, BiPAP machines can be either fixed or auto-adjusting.
- Fixed-level BiPAP: With a fixed-level BiPAP machine, pre-determined IPAP and EPAP settings are programmed into the machine and do not change at any point throughout sleep.
- Auto-adjusting BiPAP: Auto-adjusting BiPAP, or auto-BiPAP, machines automatically deliver varying EPAP and IPAP levels to accommodate different breathing patterns. This is ideal for people who are not able to tolerate the pre-set, fixed pressures that are delivered while asleep.
BiPAP devices also have several unique modes.
- Spontaneous (S): In spontaneous mode, the machine is triggered when a person breathes in or out. BiPAP-S mode may be used for people with OSA who do not respond to CPAP, those who find CPAP to be uncomfortable, or people with OSA and conditions that cause hypoventilation.
- Spontaneous/timed (S/T): The machine has a timer and will deliver a breathing cycle if a person has not taken a breath for a period of time. This setting is known as a backup rate and is typically used for people with CSA or for people whose breathing is too weak to trigger the BiPAP machine’s cycle.
- Timed (T): In this mode, the BiPAP machine delivers breathing cycles only according to a timer and not in response to a person’s breathing. BiPAP-T mode is rarely used because S/T provides the same functionality.
What Are the Benefits of BPAP?
While CPAP is effective for many, BiPAP is often recommended for people who struggle with standard CPAP settings or have more complex sleep or respiratory conditions. Benefits of BPAP compared to CPAP include:
- Easier exhalation: The lower pressure during exhale can reduce feelings of breathlessness and make it easier to fall and stay asleep.
- Better for high-pressure needs: BiPAP is more comfortable for people who require higher pressures that may be difficult to tolerate with CPAP.
- Ideal for certain conditions: BiPAP may be prescribed for central sleep apnea, complex sleep apnea, or conditions like COPD and obesity hypoventilation syndrome.
- Pressure adjustment flexibility: Some BiPAP devices offer advanced settings like backup respiratory rates or auto-adjusting pressure support, allowing for more personalized therapy.
What Are the Drawbacks of BPAP?
BPAP machines offer greater flexibility and comfort for some users, but they also come with a few potential downsides, especially when compared to standard CPAP therapy.
- Higher cost: BPAP machines are generally more expensive than CPAP devices, and insurance may require proof that CPAP was ineffective before covering BiPAP.
- Less common for standard OSA: For people with uncomplicated obstructive sleep apnea, BPAP may offer more complexity than necessary.
- More complicated settings: BiPAP machines have more customizable features, which can make setup and troubleshooting more challenging for some users.
- Noise and size: Some BiPAP models are slightly larger or louder than CPAP machines, which could be a consideration for light sleepers or frequent travelers.
Who Is BPAP Best For?
Certain BiPAP modalities are the recommended treatment for people who have a combination of obstructive and central sleep apnea. For example, BiPAP S/T is proven to effectively treat some types of central sleep apnea and can be an alternative for people who have had difficulty with CPAP therapy.
BiPAP is also the treatment of choice for central sleep apneas that are related to certain health conditions that can cause shallow or slow breathing during sleep, including:
- Central nervous system disease, such as multiple sclerosis
- Neuromuscular disease, such as muscular dystrophy
- Opioid use
- Chronic obstructive pulmonary disorder (COPD)
While CPAP therapy effectively treats obstructive sleep apnea in most people, some people may benefit from using BiPAP instead. Sleepers that require an air pressure that exceeds the pressure range available on a CPAP machine may be prescribed BiPAP as an alternative.
In some instances, people prescribed CPAP therapy struggle with treatment and are unable to continue. In other cases, CPAP therapy does not adequately treat sleep apnea. In both situations, BiPAP can be an effective alternative to CPAP.
BiPAP vs. CPAP: Which Is Best for You?
The type of PAP machine that is best for you depends on the type of sleep apnea you're diagnosed with, as well as your response to other sleep apnea treatments. Your doctor or sleep specialist will talk with you about the available options and what type of PAP therapy is best for your situation.
In general, experts agree that CPAP therapy is the best treatment for obstructive sleep apnea that isn't complicated by other health issues that affect breathing during sleep.
The best treatment for people with more complex sleep-related breathing issues, such as those with certain types of central sleep apnea, is often BiPAP. BiPAP therapy can also be a helpful option for people who cannot tolerate CPAP therapy or whose OSA does not respond to CPAP treatment.
Frequently Asked Questions
BiPAP (bilevel positive airway pressure) delivers two fixed levels of air pressure: a higher pressure when you inhale and a lower pressure when you exhale. APAP (auto-adjusting positive airway pressure), on the other hand, automatically adjusts the pressure throughout the night based on your breathing patterns, but it still delivers a single pressure level at any one time.
BiPAP is often prescribed for people who need extra support when exhaling or have conditions like central sleep apnea or COPD, while APAP is commonly used for people with obstructive sleep apnea who need variable support.
BiPAP is not considered life support. It's a non-invasive form of ventilation that helps people breathe more easily, typically used to treat sleep apnea, COPD, or other respiratory conditions. However, in hospital or emergency settings, BiPAP may be used as an alternative to invasive ventilation for people who are having serious trouble breathing. So while it's supportive, it's not classified as full life support.
You may notice BiPAP is working if you're sleeping better, feeling more rested during the day, and experiencing fewer symptoms like morning headaches, fatigue, or shortness of breath. Clinically, your doctor or sleep specialist may evaluate BiPAP effectiveness through a follow-up sleep study, machine data (such as leak rates and respiratory events), or improvements in oxygen levels and blood gas measurements.
Still have questions?
Sleep apnea products can be confusing. If you need individualized assistance, post your question to the Sleep Doctor forum.