At a Glance
CPAP, or continuous positive airway pressure, is a commonly prescribed therapy for managing sleep apnea. People may also manage their sleep apnea with bilevel positive air pressure (BIPAP), auto-adjusting positive air pressure (APAP), expiratory positive airway pressure (EPAP) and adaptive servo-ventilation (ASV) machines.
If you were recently diagnosed with sleep apnea, you may be curious about sleep apnea treatment options. A CPAP machine or other PAP device is the primary treatment offered to people with sleep apnea, and other treatment options may be available if PAP therapy fails. Learn what CPAP stands for, and how CPAP and similar machines help with sleep apnea symptoms.
Think You May Have Sleep Apnea? Try an At-Home Test

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
What Does CPAP Stand For?
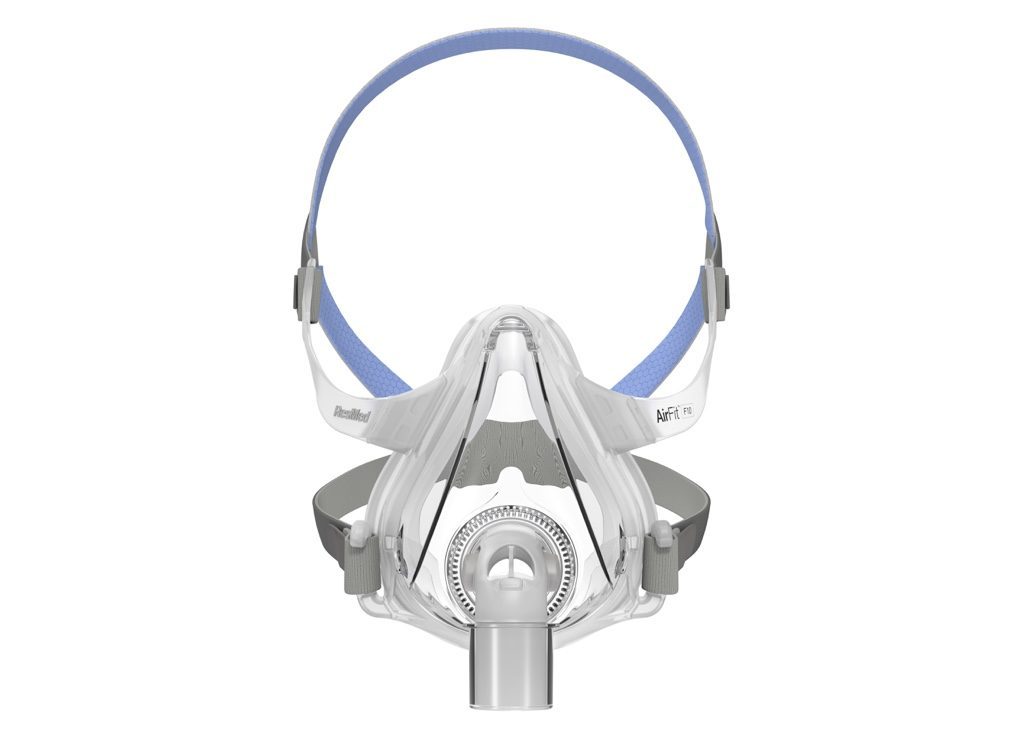
CPAP stands for continuous positive airway pressure. This long-form meaning describes the purpose of a CPAP machine, which is to continuously pressurize air to a certain level, then deliver it through a connective hose and face mask to widen the user’s airway and promote unobstructed breathing.
A CPAP machine is commonly used to treat obstructive sleep apnea (OSA) and central sleep apnea (CSA), so it is sometimes referred to as a sleep apnea machine. A sleep study or home sleep apnea test is used to diagnose sleep apnea and determine what air pressure level is needed to keep a person's airway open during sleep.
Traditional CPAP machines – also called “fixed CPAP” machines – pressurize and release air at one level. For many years, this was the most common type of PAP therapy prescribed for people with OSA. Now, several types of PAP therapy are available, and sleep specialists prescribe different types for different reasons.
What Are the Other Types of PAP Therapy?
There are multiple types of PAP therapy used to treat sleep-related breathing disorders like sleep apnea beyond CPAP. These include APAP, BiPAP, EPAP, and ASV therapies.
APAP
APAP stands for auto-titrating or auto-adjusting positive airway pressure. An APAP machine looks and works like CPAP, but does not deliver air at a fixed pressure rate. Instead, APAP devices automatically adjust air pressure levels to suit a person's needs using a proprietary algorithm. For example, an APAP machine may increase pressure when a person snores or experiences an airway blockage.
APAP, also called auto-CPAP, and fixed CPAP are the two PAP therapies most frequently prescribed first to people with OSA. In some cases, a sleep specialist may prescribe CPAP first, then offer APAP if the air pressure of a CPAP machine causes discomfort. APAP may also be preferred if a person requires different levels of air pressure at different times, such as while back sleeping or after having an alcoholic drink.
BiPAP
BiPAP, also called BPAP, stands for bilevel positive airway pressure. A BiPAP machine may look identical to a CPAP machine, but instead of delivering air at a fixed pressure rate, BiPAP releases air at two rates of pressure: a higher level while a person is breathing in and a lower level while they are breathing out.
BiPAP is usually offered to people with OSA after CPAP or APAP treatments have failed. Similarly, when CPAP doesn't work for a person with CSA, BiPAP therapy might be recommended. BiPAP may also be prescribed to people who have both OSA and another disorder, like obesity hypoventilation syndrome.
BiPAP machines can be used in spontaneous, spontaneous/timed, or timed modes, called BiPAP-S, BiPAP-S/T, and BiPAP-T. Spontaneous mode is used for people who can breathe on their own during sleep, while spontaneous/timed and timed modes are for people who cannot always begin a new in-breath on their own. Some BiPAP machines are also programmed with proprietary algorithms that allow them to auto-adjust air pressure rates, similar to APAP machines.
EPAP
EPAP stands for expiratory positive airway pressure therapy. This should not be confused with air pressure on expiration (breathing out), which also uses the EPAP acronym. All PAP devices provide some level of air pressure on expiration, but EPAP therapy refers to a specific type of machine.
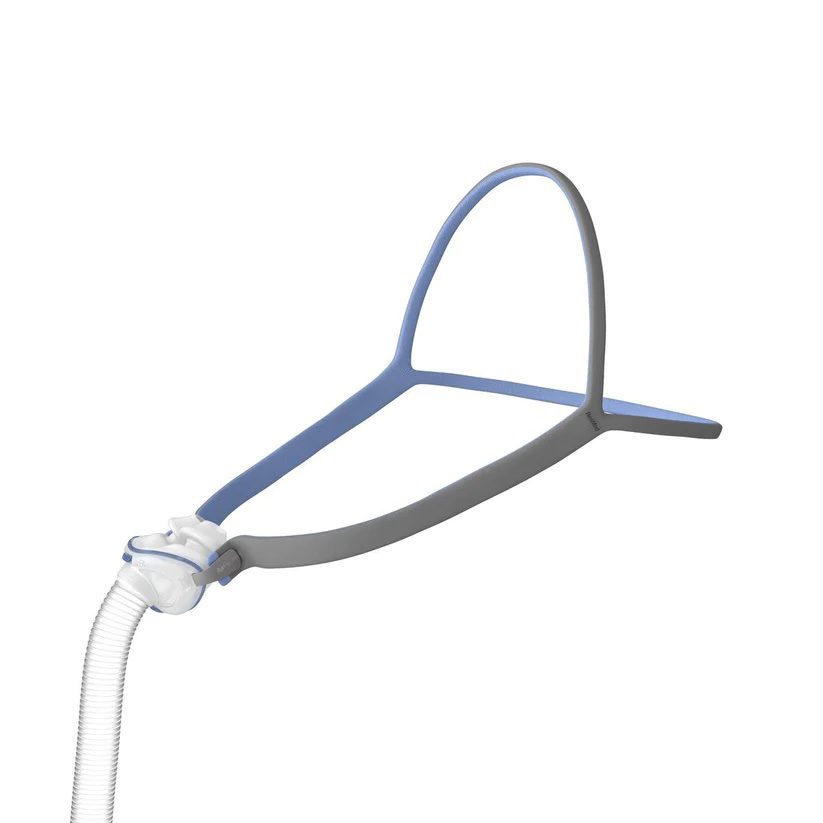
Unlike other PAP therapy devices, EPAP machines do not deliver air into the airway through a hose and mask. Instead, EPAP devices are small valves that sit in the nostrils and naturally create pressure when a person exhales during sleep without being powered by a machine. As with standard PAP machines, this pressure helps keep the airway open.
Currently, Bongo Rx is the only EPAP nasal valve device that's approved by the U.S. Food and Drug Administration (FDA) to treat OSA. Like CPAP therapy, EPAP therapy is only available with a prescription. Bongo Rx markets the device as an alternative to CPAP therapy. Although many insurance companies do not cover it, Bongo Rx is sold at significantly lower prices compared to PAP machines.
ASV
ASV stands for adaptive servo-ventilation. Like other PAP machines, ASV machines deliver air through a hose and mask into a person's airway. The air from an ASV machine has an underlying fixed pressure, like a fixed CPAP machine, but then a pattern of varying pressure rates is released as a person breathes in. ASV machines also have a back-up breathing rate that can kick in if a sleeper cannot initiate or stops initiating breathing on their own.
ASV therapy is only rarely used to treat OSA, but is more commonly used for CSA – especially after CPAP treatment has failed. ASV treatment can also be useful for people who have both OSA and CSA, those who have OSA caused by narcotics, or individuals with sleep apnea and another disorder like kidney disease.
Which Type of PAP Therapy Is Right for You?
If you've been diagnosed with sleep apnea, your doctor or sleep specialist will help you identify the best type of PAP therapy for your needs during a process called mode selection. Asking questions and reading educational materials throughout the process can help you understand the type of the therapy you've been prescribed, the best and most cost-effective way to purchase a PAP machine, and what to do if the therapy you're prescribed doesn't meet your needs.
Have a question for our experts? Submit it to the Sleep Doctor Forum.