Dry mouth is a potential side effect of continuous positive airway pressure (CPAP) therapy for sleep apnea. In CPAP therapy, a device sends pressurized air through a mask and into the upper airway to minimize breathing disruptions during sleep. For some people, this air flow can cause uncomfortable dryness in the mouth.
Various factors contribute to dry mouth, and several approaches, including use of a CPAP humidifier, may prevent or remedy this problem. We cover the key details about dry mouth, including why it happens and how to take steps to address it.
Need a CPAP Prescription? Start Here

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
Causes of CPAP Dry Mouth
CPAP-related dry mouth (xerostomia) can occur for several reasons, including as an effect of the continuous stream of air that can decrease moisture in the mouth while also reducing saliva production.
- High pressure settings: For people who use a mask that covers the nose and mouth, the steady flow of pressurized air can have a drying effect as it passes over the lining of the mouth. This effect can be even more pronounced at higher pressure settings, which deliver stronger airflow to keep the airway open.
- Dry air: CPAP air can dry out the delicate tissues in your mouth and throat. This is especially common in low-humidity environments or during colder months when indoor air tends to be drier. Without added moisture, the airflow can strip away the natural lubrication in your mouth, leading to dryness, irritation, or even a sore throat upon waking.
- Mouth breathing: Some individuals with sleep apnea naturally breathe through their mouth during sleep. In addition, some people breathe through their mouth because of nasal congestion that can arise either independently or as an effect of CPAP therapy. With more air moving through the mouth, there is a higher likelihood of oral dryness.
- Mask leak: A poor mask seal can cause air to escape during the night, especially around the mouth, which may lead to dry mouth. When a CPAP mask leaks, the machine may compensate by increasing airflow, further contributing to dryness and discomfort. Leaks can happen if the mask is the wrong size, improperly fitted, or worn out.
- Decreased saliva: CPAP therapy may interfere with moisture levels in the mouth by reducing the amount of saliva produced. Changing pressure levels in the mouth can disrupt the normal signals that trigger saliva production, leading to a higher risk of dry mouth.
- Mouth leak: When using a nasal mask, pressurized air does not flow directly through the mouth. However, air can escape or leak out through the mouth, where it can have a drying effect. For this reason, some people who use a nasal mask wear a chinstrap or mouth tape to hold their mouth closed.
How to Prevent Dry Mouth With CPAP
There are multiple ways to try to prevent dry mouth when using a CPAP machine, including by using a CPAP humidifier. Working directly with your doctor early in the process can help you find solutions as quickly as possible, including by making any necessary adjustments to your CPAP settings or accessories.
Use a Heated Humidifier
Heated humidification can go a long way toward eliminating dry mouth from CPAP therapy. Experts recommend them for most individuals who use a CPAP machine. A heated humidifier adds warm water vapor to the air that flows through the CPAP hose and mask. This moisture helps combat the drying effect of the continuous airflow from the CPAP machine.
A humidifier is integrated into most modern CPAP devices, but a separate humidifier can be attached to a CPAP machine if necessary. Some CPAP devices also have an option for heated tubing, which contributes to heated humidification and typically prevents condensation in the tubing.
To use the humidifier, make sure to fill the water chamber before going to bed. Keep in mind that CPAP manufacturers recommend only using distilled water for humidification.
It may also be worthwhile to adjust the humidity in your bedroom if you live in a dry area, such as by using a standalone room humidifier to put moisture in the air.
Make Sure Your Mask Fits Properly
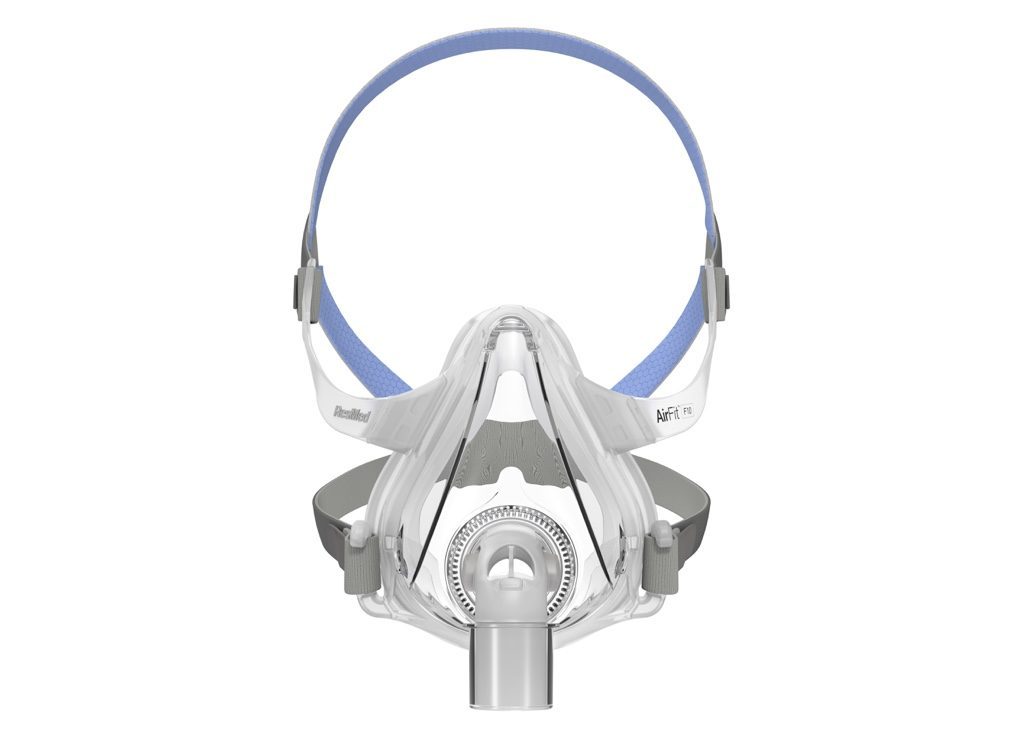
A well-fitting CPAP mask is essential for preventing air leaks that can lead to dry mouth. To get the best fit, start by selecting the right mask style and size for your face shape and sleeping position.
Use the sizing guide provided by the manufacturer and consider trying on different options if you're unsure. Once you have the correct size, adjust the headgear straps to create a snug—but not overly tight—seal. If leaks persist, check for worn-out cushions or replace the mask altogether.
Some people also benefit from switching mask styles (for example, from a nasal mask to a full-face mask) or using mask liners for a better seal.
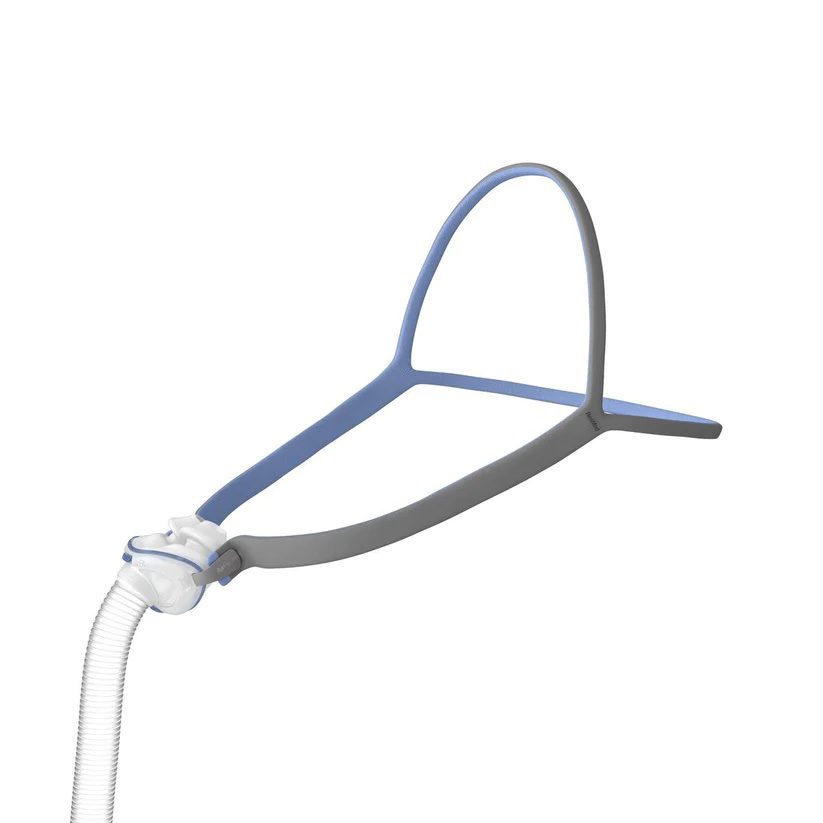
Use Mouth Tape or a Chin Strap
Keeping your mouth gently closed during sleep can help reduce dryness and improve the effectiveness of your therapy.
Mouth tape and chin straps are two common solutions. Mouth tape is a specialized, skin-safe adhesive that lightly seals the lips to encourage nasal breathing. It’s designed to be comfortable and easy to remove, helping prevent air from escaping through the mouth. Chin straps are soft, adjustable bands that wrap around the head to support the jaw and keep the mouth closed throughout the night.
Be sure to consult your sleep specialist before using mouth tape, especially if you have nasal congestion or breathing difficulties.
Try a Moisturizing Mouthwash or Spray
Using a moisturizing mouthwash or spray before bed can help relieve dry mouth symptoms and keep your mouth more comfortable during CPAP therapy. These specially formulated products coat the inside of your mouth with a protective layer that locks in moisture and soothes irritation caused by airflow.
Unlike standard mouthwashes, they’re alcohol-free and designed to reduce dryness rather than worsen it. Some sprays can also be used during the night if you wake up feeling dry. Look for products labeled for dry mouth relief and approved by dental or sleep health professionals.
Stay Hydrated
Drinking enough water throughout the day is one of the simplest and most effective ways to combat CPAP-related dry mouth. Dehydration can make your mouth feel drier and reduce the moisture available to counteract the drying effects of pressurized air.
Aim to sip water regularly during the day rather than chugging large amounts at once. Staying hydrated also supports overall health and helps your body respond better to CPAP therapy. If you're still waking up with dry mouth despite using a humidifier or mask liner, increasing your water intake may help improve symptoms.
Avoid Cigarettes and Alcohol
Smoking and alcohol use can both contribute to dry mouth and may worsen the effects of CPAP therapy. Cigarettes dry out and irritate the mouth and throat lining, reducing saliva production and increasing inflammation. Alcohol has a similar dehydrating effect and can also relax the muscles in the throat, making CPAP less effective.
For people already experiencing CPAP-related dryness, cutting back or avoiding these substances, especially in the evening, can make a noticeable difference in comfort and sleep quality. Reducing alcohol and cigarette use is also beneficial for long-term airway health and sleep apnea management.
Other Potential Causes of Dry Mouth
Using a CPAP machine is far from the only cause of dry mouth. Other medical conditions, lifestyle factors, and medications can also contribute to dry mouth.
- Nasal congestion: A stuffy nose related to allergies or infection may encourage breathing through the mouth, which can lead to mouth dryness.
- Certain medications: Treatment for various conditions can cause dry mouth as a side effect. Certain antidepressants, allergy medications, radiation therapy, and chemotherapy increase the chances of developing oral dryness.
- Chronic medical conditions: Although not always a primary symptom, dry mouth has been noted in individuals diagnosed with conditions like diabetes, autoimmune disorders, kidney failure, and thyroid disease.
- Dehydration: Dry mouth can be a consequence of dehydration, which can arise from medical conditions causing fluid loss or insufficient fluid intake during the day.
- Substance use: Frequent alcohol and tobacco use is associated with dry mouth. Both long-term smoking and alcohol consumption are believed to interfere with the body’s normal processes of producing saliva, which keeps the mouth lubricated.
More Tips for Avoiding Common CPAP Side Effects
While CPAP therapy is highly effective for treating sleep apnea, it can take some time to adjust—and some people experience mild side effects. Fortunately, most issues can be resolved with simple changes to your routine or equipment setup. Here are a few additional tips to help minimize discomfort and stick with your treatment:
- Prevent skin irritation: A properly fitted mask should feel snug but not tight. If you're experiencing red marks, rashes, or pressure sores, consider using CPAP mask liners or switching to a different mask style. Keeping your face and mask clean can also help prevent skin irritation.
- Manage nasal congestion: If you experience a stuffy nose or sinus pressure, try using a heated humidifier, saline nasal spray, or switching to a full-face mask. In some cases, nasal decongestants (used occasionally) may be recommended by your doctor.
- Reduce bloating and gas (aerophagia): Swallowing air during CPAP therapy can lead to bloating, gas, or discomfort. Lowering the pressure setting (under your doctor’s guidance) or enabling features like pressure relief during exhalation may help.
- Stop air leaks: A leaking mask can be noisy, drying, and reduce the effectiveness of your treatment. Make sure the mask fits well, clean the cushion regularly, and replace worn-out parts on schedule.
- Ease mask anxiety or claustrophobia: If wearing a CPAP mask makes you feel anxious, start by wearing it during the day while reading or watching TV. This gradual desensitization can help you become more comfortable with the sensation.
- Keep up with cleaning: A dirty CPAP machine can harbor bacteria and lead to respiratory issues. Clean your CPAP equipment, including the mask, tubing, and humidifier chamber regularly using mild soap and water, and replace disposable filters as needed.
When to See a Doctor
Your provider will schedule regular follow-ups to monitor your symptoms and response to CPAP treatment. Still, it is important to contact your doctor if dry mouth persists or if you have other issues related to sleep apnea or problems with your CPAP therapy.
Persistent Dry Mouth
If you’ve tried to reduce dry mouth but still find it to be bothersome, check in with your doctor about the most appropriate next steps.
Dry mouth may be a sign that you would benefit from a change to your CPAP mask, headgear, or device settings. Your doctor can review your CPAP setup and the steps you’ve already taken and then suggest other options for reducing dry mouth. They can also review your overall health to determine if there may be another issue causing oral dryness.
Ongoing Sleep Apnea Symptoms
Always let your doctor know if you have continuing or worsening symptoms of sleep apnea, such as excessive daytime sleepiness, frequent snoring, or difficulty concentrating. Persistent symptoms may be a sign that your CPAP therapy needs to be adjusted to more adequately treat sleep apnea.
Dental Problems
Dry mouth can impact dental health. In addition to working with your doctor, consider seeing a dentist if you notice gum irritation, bleeding, or other dental issues after starting CPAP therapy.
Concerns About CPAP Settings
You should reach out to your doctor if you have questions or concerns about your CPAP pressure settings. Although sleep specialists work to optimize settings at the outset of treatment, adjustments may be necessary.
However, you should not attempt to change the settings yourself since the pressure levels must be properly calibrated. If changes are needed, someone from your health care team can either make an adjustment for you or guide you through the process of making changes on your device.
Still have questions?
Sleep apnea products can be confusing. If you need individualized assistance, post your question to the Sleep Doctor forum.