About half of people prescribed continuous positive airway pressure (CPAP) treatment for obstructive sleep apnea (OSA) either stop using the treatment or don't use it as often as recommended. One reason a person might stop using a CPAP machine is because they experience some side effects, including skin issues like contact dermatitis.
Because untreated OSA is associated with serious health consequences ranging from an increased risk of car crashes to an increased risk of heart disease, continuing to use prescribed CPAP therapy is critical.
What Is CPAP Dermatitis?
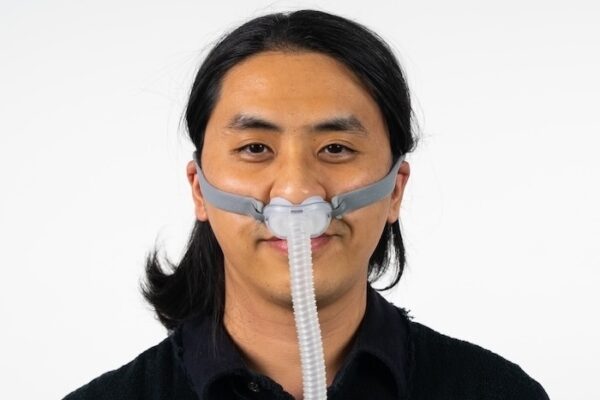
CPAP dermatitis is a type of skin irritation or rash caused by using a CPAP machine. The irritation typically develops in areas where the mask or headgear comes into contact with the skin—most often on the nose, cheeks, chin, or around the mouth.
What Are the Signs of CPAP Dermatitis?
Symptoms of CPAP dermatitis can include:
- Redness or discoloration
- Dry, flaky, or peeling skin
- Itching or burning sensations
- Small bumps or blisters
- Tenderness or soreness in affected areas
What Causes CPAP Dermatitis?
CPAP dermatitis can be caused by a variety of factors, including:
- Friction: Your CPAP mask can rub against the skin, and if it’s too tight or if you move around during sleep, this can irritate the skin and lead to dermatitis.
- Moisture: Condensation can accumulate inside the mask, creating a damp environment. Prolonged exposure to moisture can make your skin more susceptible to both contact dermatitis and infection.
- Pressure: If your mask is too tight, it will put excess pressure on certain areas of your face, such as the bridge of your nose, cheeks, and forehead. This pressure can lead to discomfort, skin breakdown, and sores.
- Poor-fitting masks: Wearing a mask that doesn’t fit properly can lead to unnecessary rubbing and pressure against your face, especially on sensitive areas like the bridge of your nose.
- Lack of proper cleaning: Regular cleaning of your CPAP mask is essential to prevent the buildup of dirt, oil, and bacteria. Failure to clean your CPAP mask regularly can lead to skin infections and irritations.
How Do You Treat CPAP Dermatitis?
Treating CPAP dermatitis involves reducing skin irritation, managing inflammation, and making adjustments to your CPAP setup to prevent future flare-ups. Here are some effective steps to help soothe your skin and stay on track with your sleep apnea therapy:
Address Inflammation
Over-the-counter hydrocortisone cream or an anti-itch lotion may help reduce redness and itching, but use these with caution and avoid applying directly where the mask sits unless advised by your doctor.
Use a Mask Liner
CPAP mask liners help reduce skin irritation by acting as a soft barrier between the mask and your skin. These liners are made from material designed to be gentle on the skin, such as cotton or moisture-wicking fabrics. Liners can also help reduce moisture.
Moisturize Before You Use Your CPAP
If you have dry skin, that could make you more likely to experience contact dermatitis from a CPAP mask. Putting on facial moisturizer, or applying a thicker cream to the areas of your face that the mask touches before going to sleep, may help.
Talk to Your Doctor
If you've tried different remedies for contact dermatitis that you believe is related to your CPAP mask and haven't had success, make an appointment with your doctor. They may be able to better troubleshoot the problem and find a solution that allows you to continue receiving your important CPAP therapy.
Can You Prevent CPAP Dermatitis?
While CPAP dermatitis can be frustrating, the good news is that it’s often preventable with a few simple habits and adjustments. By keeping your equipment clean, protecting your skin, and ensuring a proper mask fit, you can reduce the risk of irritation before it starts.
Keep Your Mask Clean
Keeping your CPAP mask clean may help with problems associated with wearing it. Experts recommend cleaning your CPAP accessories and mask using water and mild soap or distilled vinegar as frequently as the manual recommends.
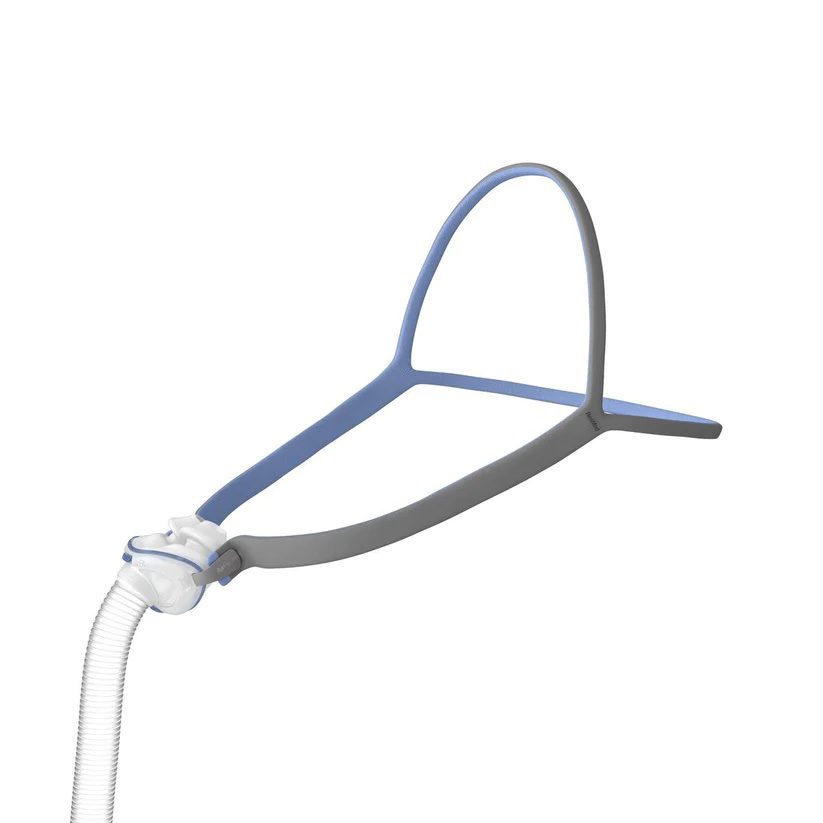
Make Sure Your Mask Doesn’t Have Any Leaks
Sometimes CPAP users experience irritant contact dermatitis because an ill-fitting mask leads to air leaks that cause dryness. If you notice air leaking from your mask, adjusting the mask's straps or trying a different style of mask may solve the problem.
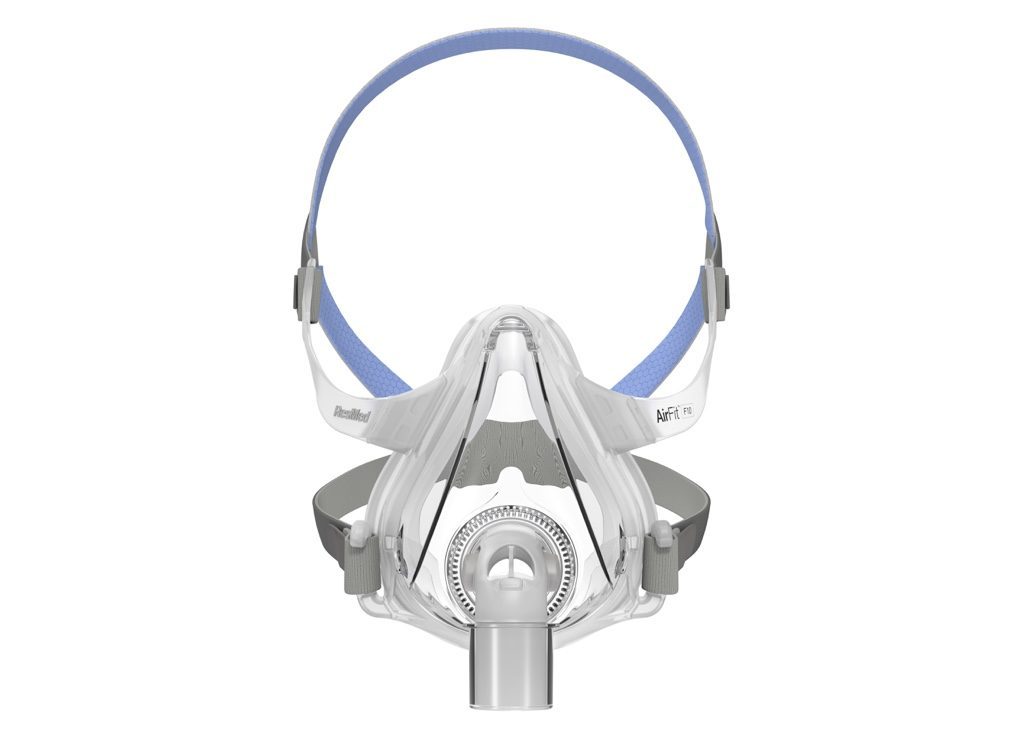
Try a Different Mask
A mask might cause skin irritation because it is too tight, too loose, or otherwise poorly fitted to a sleeper. In rare cases, something the mask is made of, like silicone or another substance, may prompt an allergic reaction. In both cases, trying a different mask type might solve the problem.