At a Glance
Continuous positive airway pressure (CPAP) machines release pressurized air at a nearly steady rate throughout the night. In comparison, auto-adjusting positive airway pressure (APAP or auto-CPAP) machines continually adjust the pressure of air based on what the device determines the sleeper needs in a given moment.
People diagnosed with sleep apnea are often prescribed positive airway pressure (PAP) therapy, which uses pressurized air airway to keep a person's upper airway open and reduce the number of breathing disruptions they have during sleep.
There are multiple types of PAP machines, and the one prescribed by a doctor depends on several factors, including the type of sleep apnea and a person's medical history. CPAP and APAP devices are the two most common PAP therapies used to treat sleep apnea.
Need a CPAP Prescription? Start Here.

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
The Difference Between APAP and CPAP
Historically, doctors prescribed CPAP therapy as the primary treatment to people with obstructive sleep apnea, the most common type of sleep apnea. In recent years, APAP therapy has become more common and is often a first-line treatment for OSA.
CPAP therapy may be prescribed to people with certain types of central sleep apnea (CSA). CSA is a type of sleep apnea in which lapses in breathing occur during sleep because the brain doesn't properly signal the breathing muscles. While other types of PAP therapy may be used to treat CSA, APAP isn't commonly used.
How CPAP Works
Traditional CPAP machines are often called fixed-level CPAPs, because the air they release flows at a relatively fixed rate of pressure throughout the night. The optimal level of air pressure is often decided during an overnight sleep study conducted in a lab but may also be determined by temporarily using an APAP machine at home.
CPAP machines may have features that change air pressure at times to increase comfort. For example, a pressure relief feature reduces pressure when a person begins exhaling to reduce the discomfort of breathing against pressurized air. A pressure ramp feature gradually increases air pressure, so a person can fall asleep before the air reaches the desired pressure.
Another CPAP feature designed to promote comfort is heated humidification. Because PAP therapy can dry out the nasal passages, heated humidification can keep the nose and mouth from becoming too dry. Heated humidification can be particularly useful for people who live in dry or cold regions, and for those who have had certain types of throat surgery.
How APAP Works
Although it looks and operates similarly to a CPAP, an an APAP machine differs in how it delivers pressurized air. Instead of releasing air at a near-constant rate, an APAP machine frequently alters the pressure of air according to a calculation by the device.
An APAP machine can sense changes in airflow to and from the lungs, such as when a sleeper's breathing has slowed or they have begun snoring. The machine then adjusts its rate of airflow accordingly, using a higher pressure of air to prevent lapses in breathing, then reducing air pressure when a higher rate is unnecessary.
Because an APAP tends to release air at a lower rate of pressure much of the time, some people may find using the machine more comfortable than using a CPAP. Like a CPAP machine, an APAP may also have additional features that add comfort, like pressure relief, pressure ramp, and heated humidification.
Why You Might Use APAP vs. CPAP
While CPAP has traditionally been the gold-standard for treating obstructive sleep apnea, APAP has recently become more commonly prescribed. A sleep specialist may opt to prescribe a person with obstructive sleep apnea an APAP machine for several reasons.
Who APAP Is Best For
- People who prefer an at-home sleep study: APAP machines can determine the necessary level of pressure from a person's home, allowing people to avoid an overnight sleep study in a lab. This is especially useful for people who have trouble undergoing a second sleep study or who have insurance that won't cover it.
- Those who find CPAP uncomfortable: Some people find an APAP machine more comfortable to use than a CPAP machine, because it generally delivers air at a lower average pressure. If a person tries a CPAP machine first and finds it uncomfortable, their provider may have them try an APAP machine instead.
- CPAP users with variable pressure needs: An APAP machine works best for people who require variable amounts of air pressure because their symptoms vary at different times. For some people, symptoms may worsen when they lie on their back, after drinking alcohol, or when they're experiencing allergies.
- Pregnant people: APAP machines are the preferred PAP therapy for pregnant people. When sleep apnea develops during pregnancy, symptoms may become more severe as pregnancy progresses. Using an APAP can continue to provide adequate treatment as needs change, without the need for another sleep study to determine optimal settings.
Who CPAP Is Best For
However, there are some instances in which sleep specialists may prescribe CPAP rather than APAP therapy.
- People with central sleep apnea: People with CSA are often treated with CPAP. There is a lack of research on whether APAP is a beneficial treatment for those with CSA.
- Those with complex sleep apnea: Complex sleep apnea describes when a person has both OSA and another disorder that impacts sleep, like heart failure or COPD. APAP isn't ideal for complicated OSA, so sleep specialists generally prescribed a fixed-level CPAP machine instead.
A Third Option: BiPAP
Bilevel positive airway pressure (BiPAP or BPAP) is another type of PAP therapy prescribed for sleep apnea. If a person with OSA cannot tolerate using a CPAP or APAP machine, their sleep specialist may have them try BiPAP. BiPAP may also be used in several circumstances for people with CSA.
A BiPAP machine looks and operates similarly to CPAP machines, but releases air somewhat differently. Instead of releasing air at a fixed rate, like CPAP, a BiPAP releases air at two pressures: one as a sleeper breathes in and another as they breathe out. BiPAP devices can also be auto-adjusting, offering a variable rate of pressure depending on a person’s needs.
Potential Side Effects of APAP and CPAP
There are several common side effects of PAP therapy and, in some instances, people with OSA can develop a form of CSA after beginning PAP therapy.
Common PAP Side Effects
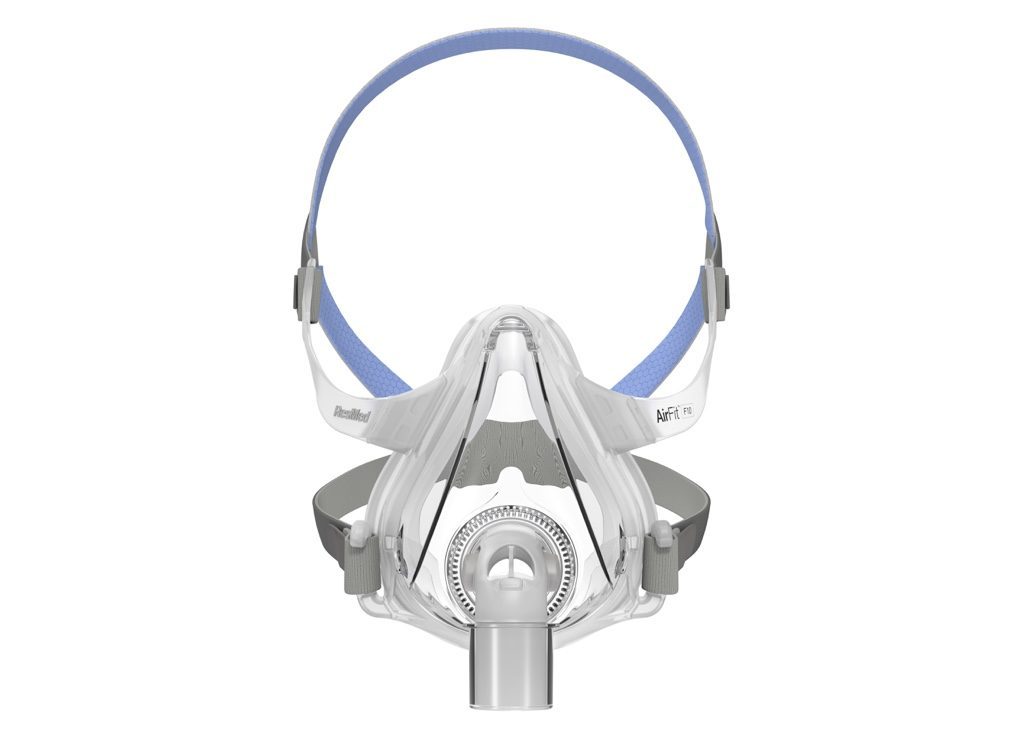
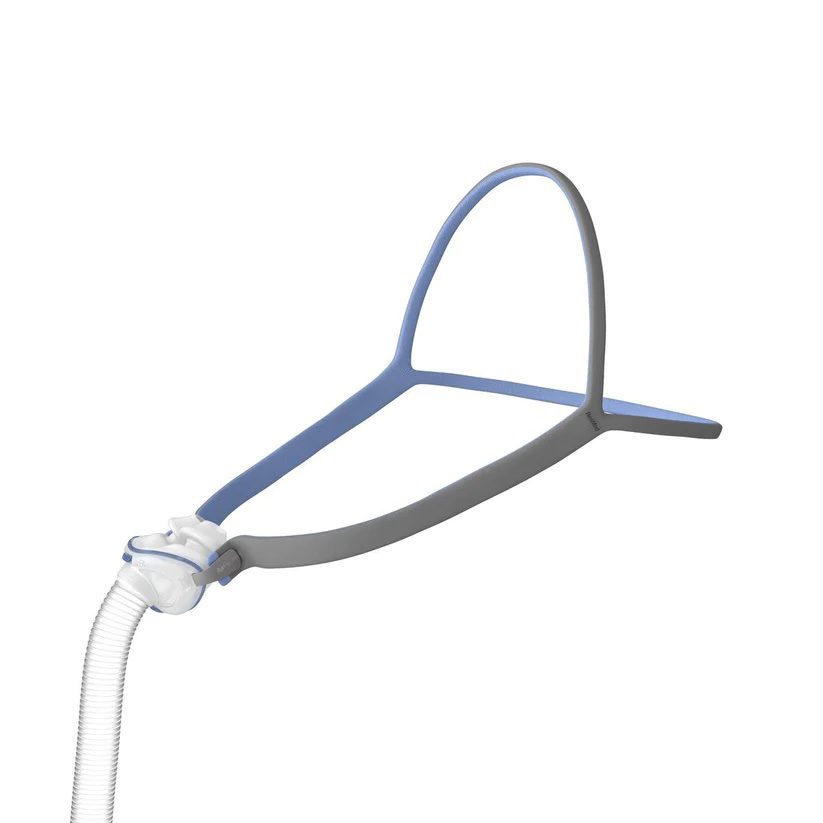
PAP therapies can produce side effects, like nasal dryness, congestion, air leaks, or feelings of claustrophobia. Each is addressed individually. For example, heated humidification can often treat dryness, while trying different mask types may reduce air leaks. Practicing wearing a mask for longer and longer periods may ease claustrophobia.
Sometimes people are tempted to not use their PAP machine enough, because they find it to be uncomfortable. For example, they might notice they are waking up more frequently in the night, swallowing air, or experiencing discomfort related to the mask or the feeling of pressurized air. In these instances, a healthcare provider can help remedy the problem and make it easier to use the device consistently.
Treatment-Emergent Central Sleep Apnea
Treatment-emergent central sleep apnea is a type of CSA that develops in 5% and 15% of people who are given PAP therapy for OSA. Certain people are more likely to develop treatment-emergent CSA, including older adults, people assigned male at birth, those with severe OSA, those with heart failure, mouth breathers, and sleepers living at a high altitude.
More than half of people with treatment-emergent CSA have it go away on its own after they continue PAP therapy for a few months. Because treatment-emergent CSA often goes away on its own, it may not require immediate treatment. If treatment-emergent CSA persists, doctors may prescribe a different type of treatment such as BiPAP.
Other Ways to Treat Sleep Apnea
Beyond PAP therapy, other treatment options for sleep apnea might be recommended depending on the type of sleep apnea and the cause of breathing disruptions.
In addition to PAP therapy, people with obstructive sleep apnea may be advised to make lifestyle changes to reduce their symptoms, including exercise, weight loss, changing sleeping positions, and cutting out alcohol and sedative use. Other treatments for OSA may include surgery, oral appliances, medication, or hypoglossal nerve stimulation.
Central sleep apnea is often treated by addressing underlying medical conditions that are contributing to breathing disruptions. People with CSA may also be treated with supplemental oxygen, medications, or phrenic nerve stimulation.
Frequently Asked Questions
For many people, APAP works just as well as CPAP at treating obstructive sleep apnea. Both devices prevent airway collapse during sleep by delivering pressurized air, but APAP automatically adjusts the pressure throughout the night based on your needs, while CPAP provides a fixed pressure. Some people may respond better to one over the other depending on their sleep patterns and pressure requirements.
Generally, APAP machines tend to be more expensive than CPAP machines due to their advanced pressure-adjusting technology. However, the cost difference isn’t always significant, and many insurance plans cover both types of devices. The added comfort and flexibility of APAP may make it a worthwhile investment for some users.
APAP may not be ideal for people with certain medical conditions, such as central sleep apnea, chronic obstructive pulmonary disease (COPD), congestive heart failure, or severe obesity-related hypoventilation.
It may also be less suitable for individuals who experience frequent air leaks or need consistent pressure due to anxiety or discomfort from changing pressure levels. A sleep specialist can help determine which therapy is most appropriate based on your specific diagnosis and needs.
Many users find APAP more comfortable than CPAP because it adjusts to your breathing patterns in real time, delivering higher pressure only when needed and lowering it when demand decreases. This can make it easier to fall asleep and stay asleep.
However, comfort is subjective; some people prefer the consistent airflow of a CPAP machine. Proper mask fit and pressure settings play a major role in overall comfort with either option.
Still have questions?
Sleep apnea products can be confusing. If you need individualized assistance, post your question to the Sleep Doctor forum.