Approximately 20% of American adults have obstructive sleep apnea (OSA), a disorder which causes repeated pauses in breathing during sleep. Continuous positive airway pressure (CPAP) therapy is one of the most common ways of treating OSA.
To get the most out of CPAP therapy, it's helpful to know how CPAP machines work, how they can help people with sleep-related breathing problems, and how to troubleshoot some of the challenges that may arise when using a CPAP machine.
Need a CPAP Prescription? Start Here.

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
What Is a CPAP Machine?
A CPAP machine is a medical device that creates a stream of pressurized air to keep a person’s airway open and encourage stable breathing as they sleep. It’s one of the most common and effective tools used to treat sleep-related breathing disorders like obstructive sleep apnea.
Parts of a CPAP Machine
- Machine: The machine includes controls for operating the device, as well as a motor that generates the stream of pressurized air.
- Air filter: This component filters the air generated by the CPAP machine.
- Hose: A long tube connects directly to the CPAP machine and carries air to the mask.
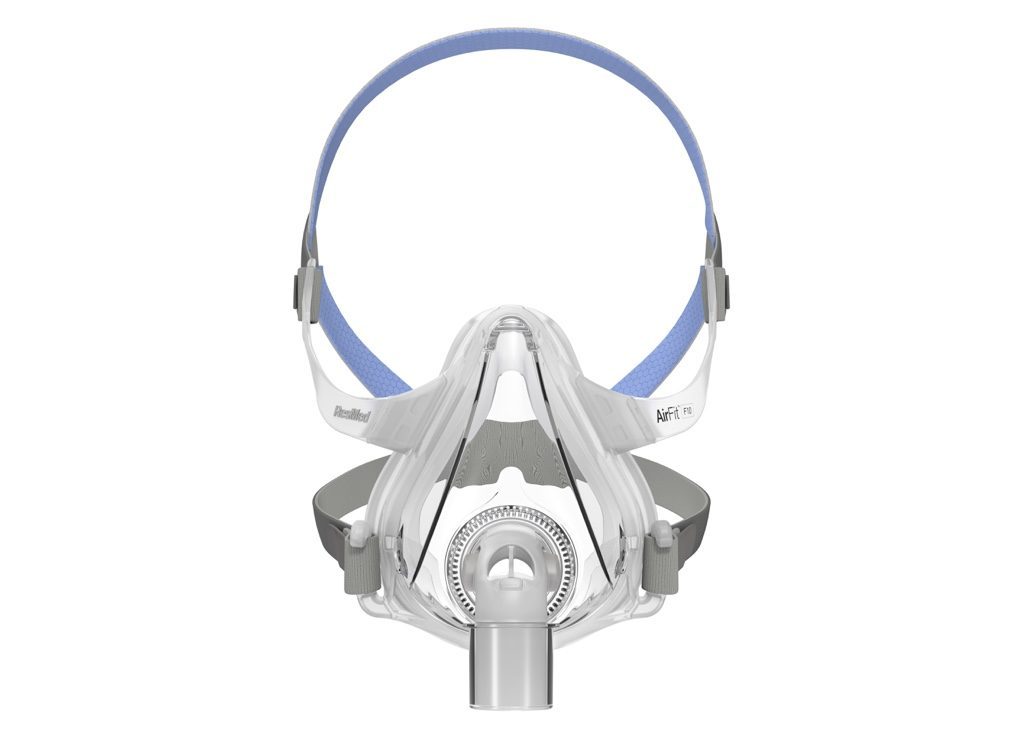
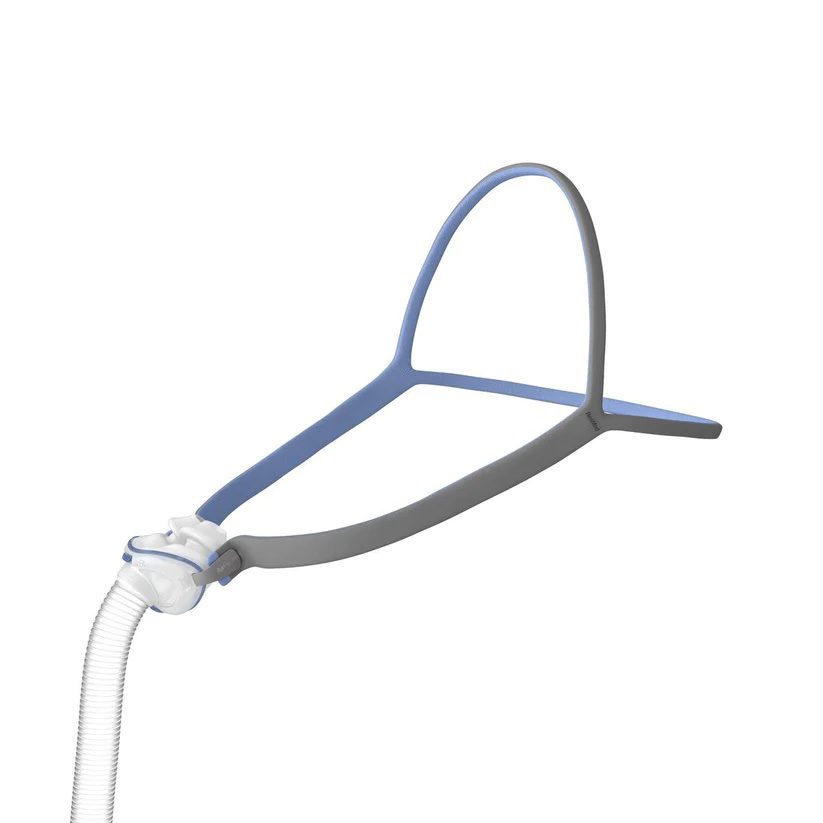
- Mask: The mask delivers the pressurized air into the nose and/or mouth so that the airway is kept open for normal breathing during sleep. There are many styles of CPAP masks, and they typically include straps to hold the mask in place.
- Humidifier: Most CPAP devices have a heated humidifier that uses water from an attached reservoir to add moisture to the air to reduce discomfort and dry mouth caused by the stream of pressurized air.
CPAP, APAP, and BiPAP
There are several kinds of positive airway pressure (PAP) therapy. Important differences between them relate to how these devices deliver pressurized air to keep the airway open.
- Continuous positive airway pressure (CPAP): A CPAP machine uses a consistent level of air pressure that's the same for inhaling and exhaling.
- Bilevel positive airway pressure (BiPAP or BPAP): A BiPAP machine has two pressure levels, one for when a person inhales and another for when they exhale.
- Auto-titrating positive airway pressure (APAP): Sometimes called an adjustable PAP, or auto-CPAP, these devices can automatically modify pressure levels in response to a person’s breathing. In most cases, that pressure level is the same for both inhalation and exhalation.
For most people with obstructive sleep apnea, CPAP is recommended as the initial treatment. However, if CPAP isn't effective or if someone has certain lung diseases or other coexisting health conditions, a different type of PAP device may be prescribed.
Types of CPAP Masks
- Nasal masks: A nasal mask fits around the perimeter of the noses and conducts the pressurized air through the nasal passages.
- Nasal pillows: Instead of going over the nose, a nasal pillow mask or nasal cradle mask sits under the nose and above the upper lip. Nasal pillow masks may have two flexible silicone prongs that seal just inside the rim of each nostril to deliver the pressurized air from the CPAP machine. A nasal cradle mask sits at the base of the nose, with a flexible silicone opening that seals around the nostril openings to conduct air into the nasal cavity.
- Full face (oronasal) mask: This type of mask goes over both the mouth and the nose. Often, an oronasal mask covers an area from the bridge of the nose to the bottom of the mouth. Some oronasal masks go over the mouth while using a nasal pillow to deliver air through the nose.
What Does a CPAP Machine Do?
A CPAP machine works by delivering a continuous stream of pressurized air through a mask and tubing system while you sleep. This steady airflow creates a cushion of air that helps keep the upper airway open, preventing it from narrowing or collapsing.
When the airway remains open, breathing becomes smoother and more consistent, reducing snoring and preventing the pauses in breathing that occur with OSA. The air pressure level is prescribed by a sleep specialist and may be adjusted for comfort or effectiveness.
What Is a CPAP Machine Used For?
A CPAP machine is primarily used to treat obstructive sleep apnea. In addition, CPAP therapy may also be prescribed for related conditions such as upper airway resistance syndrome (UARS) or certain cases of central sleep apnea when combined with advanced pressure settings.
Consistent CPAP use has been shown to improve daytime alertness, reduce snoring, and lower the risk of serious health problems linked to untreated sleep apnea, including high blood pressure, heart disease, and stroke.
Benefits of CPAP Machines
Regular use of a CPAP machine can often reduce or resolve symptoms of obstructive sleep apnea, improving sleep and a patient’s quality of life. Specific benefits of CPAP use include:
- Reduced snoring
- More consistent breathing during sleep
- Less daytime sleepiness
- Healthier blood pressure
- Improved focus and memory
- Enhanced mood
- Better sleep for a bed partner
- Fewer morning headaches
In most cases, it takes several weeks to notice these benefits, but some people find that their sleep improves almost immediately after starting CPAP therapy.
Side Effects of CPAP Machines
CPAP therapy can provide important health benefits, but it can also cause side effects. For many people, getting accustomed to sleeping with a CPAP machine can be challenging. It often takes days or weeks to get used to using a CPAP machine through the night.
Some side effects that may arise when using CPAP therapy include:
- Discomfort from the mask or stream of pressurized air
- Nasal congestion, dryness, irritation, or nosebleeds
- Claustrophobia or anxiety when wearing the CPAP mask
- Dry mouth
- Skin irritation, especially around the mouth and nose
In many cases, practical steps or adjustments of CPAP settings can resolve these side effects and make nightly CPAP use significantly more comfortable. Anyone who experiences one or more of these issues should work closely with their health care team to improve their experience with CPAP therapy.
Troubleshooting Common CPAP Problems
Starting CPAP therapy can take some adjustment, and it’s normal to experience a few challenges along the way. Issues like mask leaks, dryness, or discomfort can interfere with consistent use, but most of these problems have simple solutions.
High CPAP Pressure
For some people, the constant flow of pressurized air can be uncomfortable. Several approaches can help manage a feeling of excess air pressure.
- Ramp function: CPAP devices may offer a ramp feature that starts the night with a lower pressure level that builds up over time. This allows a person to fall asleep while the air pressure is lower and less bothersome.
- Pressure relief setting: Some CPAP devices include a pressure relief setting that slightly decreases the air pressure when a person exhales.
- Changing devices: If the steady air pressure of a CPAP isn't tolerable, a doctor may consider switching to a type of PAP device that has more variability in the pressure levels.
Having the right pressure level is important to properly treating obstructive sleep apnea, so it's important to work with a doctor before making any changes to a CPAP device’s pressure settings.
Uncomfortable CPAP Mask
It can be hard to find a CPAP mask that can be worn comfortably throughout the night. For people struggling with their mask, it can be helpful to work with their health care team to consider other mask options.
Masks come in many different styles and shapes. The placement of the straps and type of padding can affect how it feels. With so many options available, many people will need to try out a number of masks before finding the one that works best for them.
Claustrophobia While Wearing a CPAP Mask
A few different solutions may help if wearing the CPAP mask creates feelings of claustrophobia.
- Mask desensitization: This approach involves putting on the mask during waking hours and practicing while doing something relaxing. The amount of time wearing the mask should be minimal at first and then gradually increase as a person gets acclimated, eventually using the CPAP mask through the night. Be sure to disconnect the CPAP tubing from the mask if you're practicing without the machine on.
- Switching masks: The feeling of claustrophobia may be reduced by changing to a smaller mask or one that has a different profile on the face.
- Relaxation exercises: Learning and practicing relaxation techniques may decrease the anxiety that can come from putting on the mask. Activities such as journaling, meditation, listening to music, or stretching before bed can promote a calm state of mind that enhances sleep quality.
Waking Up With Dry Mouth or Nasal Congestion
Mouth breathing can lead to dry mouth in people who use nasal CPAPs, and this problem may be addressed by using a chin strap that keeps the mouth closed during sleep. People using a full face or an oronasal mask can try using the heated humidifier or turning up the humidifier setting on their CPAP machine to reduce dry mouth.
CPAP masks may also contribute to nasal congestion. Prescription medications may help with this congestion, and for some people, the problem may be resolved by switching to a mask that covers both the mouth and nose.
CPAP Air Leaks
Air leaks occur when the pressurized air from the CPAP doesn't reach the airway at the back of the throat. This may occur if the mask doesn't create a tight seal on the face or if a person breathes through their mouth while using a nasal CPAP.
When air leaks occur, they can be addressed by changing the type or shape of the mask. People using a nasal mask can try using a mask with a chin strap that prevents the mouth from opening during the night.
Facial Hair Interfering With CPAP Mask
Tips for people whose facial hair is affecting the fit of a CPAP mask include:
- Switching to a mask with a different shape
- Using a different kind of mask, such as a nasal pillow mask
- Trimming or shaving facial hair
- Using a cloth mask liner or a mask with a memory foam cushion
CPAP Mask Irritating Skin
If a mask or its straps are pressing too firmly against the face, it may cause skin irritation. Dirty masks or old masks may also cause inflammation, skin breakouts, or sensitivity. CPAP masks shouldn't cause skin breakdown or sores on the face or scalp. Practical steps to reduce skin problems from a CPAP mask include:
- Cleaning the mask regularly
- Adjusting straps to avoid having the mask too tight or too loose
- Switching to a different type or size of mask
- Trying one or more types of padding or cushions to reduce pressure on the skin
CPAP Noise
Although modern CPAP devices have become quieter, the noise may be bothersome to some people or their bed partner. Keeping the machine under the bed, adjusting the machine’s alarm settings, adjusting the mask, or wearing earplugs can often decrease noise disruptions.
If noise continues to be a problem, a doctor can help address whether there's a problem with the CPAP machine or whether another model of CPAP can offer quieter performance.
CPAP Cleaning and Maintenance
CPAP devices usually come with specific instructions for cleaning and maintenance, and it's important to follow these directions and any guidance given by the doctor.
Some parts of the CPAP, such as the mask, may need to be cleaned daily, while other parts may need a thorough cleaning and disinfecting on a weekly basis.
In addition, it's important to watch for wear and tear of CPAP components and to replace them when necessary. Masks, straps, and hoses should be replaced periodically based on the manufacturer’s instructions. These items should also be discarded if the material becomes noticeably dirty or damaged.
When to Talk to Your Doctor
CPAP therapy must be prescribed by a doctor. A doctor or sleep specialist may help select a device, determine the right pressure level, suggest certain settings, and recommend a type of mask. During this process, patients can communicate any preferences they have about specific components of their CPAP setup, including the mask.
When beginning CPAP therapy, it's critical to stay in regular contact with the doctor about any problems or challenges that arise. In many cases, the doctor can suggest strategies to manage or overcome difficulties so that the device can be used every night to treat sleep apnea.
Over time, patients should continue to check in with the doctor about how their CPAP treatment is going and raise any new issues that may have developed. The doctor may use data collected by the CPAP machine to make sure that the mask and device are functioning properly and to see how well the treatment is working.
Have a question for our experts? Submit it to the Sleep Doctor Forum.Frequently Asked Questions
CPAP stands for continuous positive airway pressure. While there are multiple types of positive airway pressure (PAP) devices, the term “continuous” reflects that a CPAP uses a consistent level of air pressure for both inhaling and exhaling.
CPAP devices are only available by prescription. People who think they may have obstructive sleep apnea or another breathing condition that could be helped by CPAP therapy should speak with a doctor or sleep specialist.
If a CPAP machine is prescribed, the doctor will determine the appropriate level of pressure and may help identify a provider who can supply the CPAP device, mask, and other accessories.
The cost of a CPAP machine depends on the brand and model that is prescribed as well as a person’s insurance coverage.
Health insurance may cover some or all of the costs of CPAP therapy for people who are diagnosed with obstructive sleep apnea. However, coverage and out-of-pocket costs can vary significantly based on the details of the insurance plan, including whether there is a deductible.
Without insurance, a CPAP device may cost several hundred to over a thousand dollars, along with recurring costs from replacement components like masks and tubing.
Some insurance companies require at least four hours of CPAP usage to provide coverage for the cost of the machine and parts. From a medical perspective, using CPAP treatment throughout the sleep period is advisable to support normal breathing and avoid consequences associated with sleep disruption and fluctuations in blood oxygen levels.
Studies have found that using CPAP for a minimum of four hours per night can reduce daytime sleepiness and generate other health benefits. These benefits can be increased by using the CPAP device for more time during the night.
People with obstructive sleep apnea whose jobs require daytime alertness, such as commercial truck drivers and pilots, have minimal use requirements for CPAP in order to continue performing their work in compliance with safety standards.
It's best to use CPAP during any period of sleep, so people with sleep apnea are encouraged to use their CPAP machine during afternoon naps.
Breathing disruptions from obstructive sleep apnea will return during sleep after stopping CPAP use. Problems like daytime sleepiness and elevated blood pressure can develop within two weeks after CPAP use is stopped or significantly reduced.
For these reasons, it is important for anyone who is having problems sticking with CPAP therapy to work proactively with their doctor to address those challenges and make it easier to consistently use their CPAP device.
CPAP therapy is a common initial treatment for obstructive sleep apnea, but it is just one of several treatment options. Depending on a person’s situation, treatments options other than CPAP may include:
- Other types of PAP therapy
- Mouthpieces and oral appliances that change the positioning of the tongue or jaw
- Surgery to remove tissue around the upper airway
- Surgery to implant a device that stimulates nerves that help control the opening of the airway
These alternatives to CPAP therapy are not viable for all people with obstructive sleep apnea, and questions about the most appropriate treatment for sleep apnea should always be discussed with a doctor.
Still have questions?
Sleep apnea products can be confusing. If you need individualized assistance, post your question to the Sleep Doctor forum.