At a Glance
Medicare may contribute to the cost of sleep studies when they’re deemed medically necessary to diagnose sleep disorders such as sleep apnea. Coverage depends on the type of sleep study performed and whether you meet Medicare’s eligibility and documentation requirements.
Sleep studies can be an important step in diagnosing conditions like sleep apnea, but many people worry about the cost and whether Medicare will cover them. Coverage depends on factors such as medical necessity, the type of sleep study performed, and which parts of Medicare you have. This guide explains what Medicare covers, eligibility requirements, and potential out-of-pocket costs.
Think You May Have Sleep Apnea? Try an At-Home Test

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
Does Medicare Cover a Sleep Study?
Medicare contributes to the cost of sleep studies where these are considered medically necessary. This includes when sleep studies are ordered as part of the diagnostic process for certain sleep disorders or to analyze if CPAP or another therapy is helping treat symptoms of your sleep disorder.
Sleep studies fall into one of four categories according to how many metrics they measure. The most comprehensive type is a type I sleep study, also called polysomnography. Polysomnography monitors brain waves to analyze sleep stages. The test also measures your eye movements, heart rate, airflow, breathing, and blood oxygen levels. This type of sleep study is typically performed in a sleep lab with a technician on hand.
Type II, III, and IV sleep studies measure fewer variables and may take place outside of a sleep lab. These tests are mostly used for diagnosing clearcut cases of moderate to severe sleep apnea. Medicare covers type I, II, III, and IV sleep studies under Medicare Part B. If you have Original Medicare, you’ll generally pay 20% while Medicare covers 80% of the Medicare-approved cost.
Medicare only starts to pay once you reach your deductible, which is $283 in 2026. You also need to pay your monthly Part B premiums to remain eligible, whether or not you make any claims.
For providers who don’t accept assignment, your out-of-pocket costs may be higher. By contrast, your out-of-pocket costs may be lower if you have extra coverage through Medigap or Medicare Advantage (Part C).
What Conditions Are Covered?
Sleep studies are helpful for diagnosing sleep disorders that depend on certain measurements, like your heart rate or breathing. However, not all sleep disorders can be diagnosed with a sleep study. Accordingly, Medicare only offers coverage for conditions where a sleep study forms an integral part of the diagnostic process. These conditions are:
- Obstructive sleep apnea
- Narcolepsy
- Impotence
- Parasomnias including sleep walking, rapid eye movement sleep behavior disorder (RBD), or violent sleep terrors
As a general rule, Medicare doesn’t offer coverage for other sleep disorders such as insomnia or circadian rhythm sleep disorders. Medicare may deny coverage for a sleep study if you have a very clear case of sleepwalking that doesn’t pose any physical danger. Also, Medicare won’t pay for a test that only uses actigraphy to track your limb movements during sleep, unless this is performed as part of a sleep test.
If you’re diagnosed with obstructive sleep apnea, Medicare may also cover the cost of CPAP therapy.
Does Medicare Cover a Sleep Study at Home?
Medicare offers coverage for at-home sleep studies if you have already been thoroughly assessed by a doctor and they’ve determined you’re very likely to have moderate to severe obstructive sleep apnea. In this case, Medicare also covers the cost of the doctor’s services.
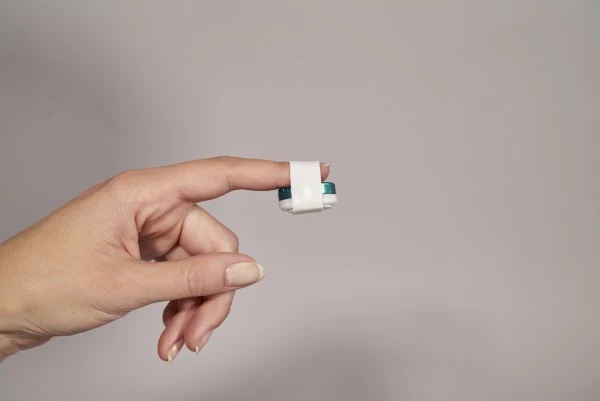
Home sleep apnea tests are more affordable and accessible than in-lab tests, and many people find it more comfortable to perform the test in the comfort of their own bedroom. Most are type III or type IV tests that you can set up by yourself.
To ensure Medicare coverage, you must use a Medicare-approved test, and a qualified physician must give you clear instructions on how to use it. You’ll need to document details like start time and study duration, and the test must gather data relevant metrics including airflow.
Home sleep testing is currently only adequate for diagnosing moderate to severe OSA, so testing for parasomnias or narcolepsy or screening in people with no symptoms wouldn’t qualify for Medicare coverage. Medicare also won’t cover the cost of an at-home sleep test if you have certain coexisting conditions, such as lung disease or congestive heart failure.
How Often Will Medicare Pay for a Sleep Study?
Medicare covers maximum two polysomnography studies or one home sleep study per year, unless there’s a very good reason you need additional studies. Medicare can either cover a second polysomnogram to help with CPAP titration or a split-night study in which the first half of the study is used to diagnose obstructive sleep apnea and the second half is used to set up your CPAP pressure settings.
Where necessary, Medicare will also cover a follow-up sleep study to evaluate your response to sleep apnea treatment — whether CPAP therapy, an oral appliance, or surgery — especially if your treatment doesn’t seem to be working. You may also be eligible for coverage of a new sleep study to readjust your CPAP machine settings if you’ve recently gained or lost a lot of weight.
Do Sleep Studies Expire for Medicare?
Providers who accept assignment are responsible for filling out the appropriate forms at the time of the study and billing Medicare directly. If your provider doesn’t submit the claim for you, you may need to submit it yourself within 12 months of having done the sleep study to remain eligible for Medicare coverage.
Sleep studies are usually performed with the specific aim of diagnosing a medical condition or evaluating whether a treatment is working. While they don’t expire per se, the results may no longer be useful if you don’t pursue the next steps soon after performing the test. Medicare generally covers the cost of a new sleep study if it’s deemed medically necessary and your last sleep study was performed more than one year prior.
Medicare Sleep Study Requirements
Obtaining Medicare coverage for a sleep study follows a similar process to other Plan B claims. You’ll need a referral from your doctor, as well as documented medical evidence (such as results from a medical exam or lab test) that shows you need to get these tests to diagnose a sleep disorder.
If you get the sleep study done in a clinic, it must be a certified clinic run by qualified medical professionals. For both sleep studies and polysomnography, the attending physician must be board-certified or belong to a sleep center with appropriately credentialled staff, and the technician must hold relevant qualifications. Full polysomnography (a type I test) is only covered if it’s carried out in a permanent sleep lab.
As long as you’re up-to-date on your premiums and you’ve met your deductible for the year, Medicare coverage will kick in and cover 80% of the Medicare-approved cost. Your doctor should handle the paperwork if they accept assignment, or you may need to submit the reimbursement claim yourself if not.
Have a question for our experts? Submit it to the Sleep Doctor Forum.