Look & Feel
While not as streamlined as some at-home sleep apnea tests, the ApneaLink Air has a simple belted design with indicators to help users set it up correctly.
Ideal For
- People whose doctors prescribe this at-home test
- Adults with symptoms of moderate to severe sleep apnea
- Those who cannot easily get to a sleep clinic
Who Should Keep Looking
- Children with symptoms of sleep apnea
- People who would prefer to directly purchase their own sleep apnea test rather than going through their provider
- Anyone with symptoms of sleep disorders other than sleep apnea
-
Price
Varies
-
Test Location
Chest, nasal, & finger
-
Warranty
2 years
-
Weight
Recorder weight: 2.3 oz
Sleep breathing disorders like obstructive sleep apnea (OSA) and central sleep apnea (CSA) are usually diagnosed after a sleep study at a clinic. However, at-home sleep apnea tests like the ResMed ApneaLink Air are an alternative diagnostic tool that allow certain patients to be tested while sleeping in their own bed.
The ResMed ApneaLink Air is a sleep apnea test that is usually prescribed by a medical professional. The test tracks up to five metrics that allow doctors to diagnose sleep apnea and differentiate between OSA and CSA.
We’ll explain what you should know about the ResMed ApneaLink Air test, including how it works, how to set it up and use it, and how it compares to other at-home sleep apnea tests and in-clinic sleep studies.
Use this SleepApnea.org link for the most current discount on ResMed products
Shop NowWhat Is Obstructive Sleep Apnea (OSA)?
The term sleep apnea refers to conditions that cause pauses in breathing, called apneas, during sleep. OSA is the most common type of sleep apnea, and it affects up to 30% of men and 15% of women in the U.S.
People with OSA experience apnea events due to a collapsed or blocked airway, usually caused by relaxed muscles and tissue.
Men, people with a higher body mass index (BMI), and smokers all have a greater risk of developing OSA. The shape of a person’s jaw and the size of their tonsils can also make them more likely to develop OSA.
Doctors use a scale called the apnea-hypopnea index (AHI) to diagnose OSA and understand its severity. An AHI score is calculated by dividing the number of apnea events a person experiences in one night by the number of hours they have slept.
| Sleep Apnea Severity | AHI Score |
|---|---|
| Normal Breathing | 0-4 |
| Mild OSA | 5-15 |
| Moderate OSA | 15-30 |
| Severe OSA | 30+ |
Signs and symptoms of OSA: Since the symptoms can be subtle, OSA often goes undiagnosed. It may be worth speaking to your doctor about sleep apnea if you experience symptoms such as:
- Snoring, especially when accompanied by gasping, snorting, or choking sounds
- Waking up frequently during the night
- Increased nighttime urination
- Inability to concentrate
- Dry mouth and headaches when you wake up
- Sexual dysfunction
- Irritability and other mood changes
- Excessive daytime sleepiness, even when you have slept well
How the ApneaLink Air Detects Symptoms of Obstructive Sleep Apnea
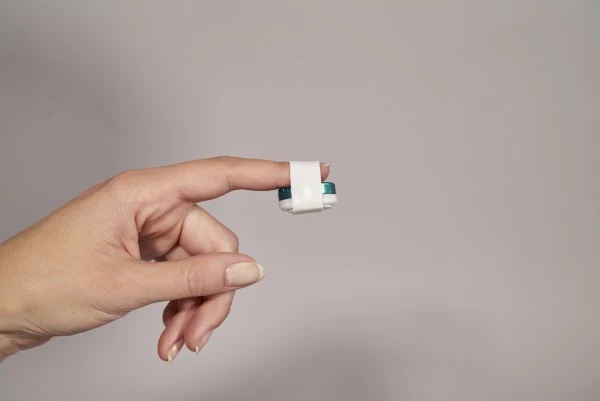
The ApneaLink Air uses a central device as well as an effort sensor, fingertip oximeter, and nasal cannula to track up to five different metrics. Your doctor can use this data to help with diagnosis of OSA or CSA.
Respiratory effort:
The effort sensor allows your doctor to see whether you are attempting to breathe during an apnea event. This information helps them determine whether you are experiencing OSA or CSA.
Respiratory flow:
The test can detect subtle apnea events by comparing your respiratory effort with the amount of air you inhale through your nose.
Snoring:
Loud snoring is a common symptom of sleep apnea, but doctors can also determine its severity and correlation to sleep apnea based on how much time you spend snoring.
Blood oxygen saturation:
The ApneaLink Air’s fingertip oximeter detects the amount of oxygen in your blood. This is an important metric since your blood oxygen levels are lower during an apnea event.
Pulse:
Apnea events cause a characteristic slowing and speeding up of your heart rate that the test can monitor via your pulse.
Types of Sleep Apnea This Device Detects
The ApneaLink Air offers doctors the information they need to diagnose both OSA and CSA. It can also detect Cheyne–Stokes respiration, a breathing pattern that can indicate heart failure.
If your doctor believes you have symptoms of other sleep disorders, they may recommend that you complete a sleep study at a clinic.
The ApneaLink Air’s Accuracy at Detecting OSA Symptoms
At-home tests like the ApneaLink Air have been shown to effectively detect moderate to severe sleep apnea. However, in-clinic sleep studies remain the gold standard for accuracy and may be a better choice for people with mild sleep apnea symptoms.
The ApneaLink Air uses lights to indicate a good signal during set-up, potentially limiting user errors that can affect the test’s accuracy.
How This Device Stacks Up Against Traditional Sleep Studies
A sleep study conducted at a sleep clinic is the traditional way of diagnosing sleep apnea. While at-home sleep apnea tests like the ApneaLink Air can be an effective alternative for some people, each approach has benefits and drawbacks.
Even if your doctor says you are a good candidate for at-home sleep apnea testing, it’s important to consider which type of testing best suits your needs.
ApneaLink Air vs. In-Lab Sleep Studies
Your doctor may recommend an in-lab sleep study if you exhibit symptoms of other sleep disorders or if you have health conditions that may require further monitoring during the study.
| ApneaLink Air | In-Lab Sleep Study |
|---|---|
Benefits:
| Benefits:
|
Limitations:
| Limitations:
|
Does the ApneaLink Air Replace a CPAP Titration Study?
The ApneaLink Air does not replace all in-lab studies, as diagnosis is not the only reason someone with sleep apnea may need to attend a sleep clinic.
Continuous positive airway pressure (CPAP) therapy, the most effective treatment for OSA, uses pressurized air to keep the user’s airway open during sleep. People who use a CPAP machine or a bilevel positive airway pressure (BiPAP or BPAP) machine must undergo a CPAP titration study to determine the correct level of air pressure for their needs.
Some people with sleep apnea use an automatic positive airway pressure (APAP) machine, which monitors the user’s breathing to determine the correct air pressure level. If your doctor believes an APAP machine would work for your needs, you may be able to do the initial titration at home.
Is This At-Home Sleep Apnea Test FDA Approved?
The ResMed ApneaLink Air was approved by the U.S. Food and Drug Administration (FDA) in 2015 as a ventilatory effort recorder.
What You Need to Know About the ResMed ApneaLink Air
The ResMed ApneaLink Air uses sensors to record data that your doctor can use to help confirm a diagnosis of OSA and CSA.
Unlike some at-home tests, the ApneaLink Air cannot be purchased by the general public and is usually provided to users by a health care professional. The device must then be returned to your doctor so that they can access your data and use it to formulate a diagnosis.
What Comes With It
The ApneaLink Air consists of a central device and several reusable and disposable sensors that your doctor may or may not include. The test also comes with the belt and clips needed to secure the sensors. Users may want to purchase medical tape to further secure any loose cords.
Components:
- ApneaLink Air device
- Belt
- Nasal cannula
- Effort sensor
- Oximeter belt clip
- Oximeter cord
- Disposable oximeter finger sensor
- Reusable oximeter finger sensor
- Carry bag
Technical Specifications
The metrics recorded by the ApneaLink Air allow doctors to determine whether the user has OSA or CSA, including information on whether the user’s sleep apnea is related to their sleep position. Cheyne-Stokes respiration detection also lets doctors know when they should investigate other causes for disordered breathing.
The ApneaLink Air also includes features that simplify the setup and testing process, such as sensor connection indicators and a test-complete light.
Features:
- Records up to five metrics
- Calculates AHI depending on the user’s sleep position
- One-touch start and stop button
- Up to 48 hours of recording time
- Indicators to signal a good connection with sensors
- Test-complete light
- Can differentiate OSA from CSA
- Can detect Cheyne-Stokes respiration
- After the test is complete, a circular indicator divided into 25% increments provides an assessment of data quality.
How to Use This Device
The ApneaLink Air comes with written instructions, and instructional videos are available online. If you have any questions or concerns about setting up and using this test, your doctor is the best source for further information. They may also be able to walk you through the process before you leave with the device.
Step 1:
The ApneaLink Air requires two AAA batteries to function. Once the batteries are installed, slide both the device and the effort sensor onto the belt as shown in the instruction booklet.
Step 2:
Next, unscrew the protective cap on the end of the nasal cannula, insert the end into the device as indicated, and turn clockwise until the connector is firmly in place.
Step 3:
The effort sensor can be connected to the device by removing the protective cap, inserting the end into the device as indicated, and turning it clockwise until it’s secure.
Step 4:
Attach the fingertip sensor to the oximeter cable. Once this is done, attach the belt clip to the oximeter. Then you should be able to push the cable into the device.
Step 5:
Put on the belt by slipping the end of it through the free slot on the effort sensor. Make sure that the belt is secure but not too tight across the center of your chest.
Step 6:
Attach any additional accessories you have as indicated in the written instructions. All accessories should be secure but not too tight.
Step 7:
To start the test, press and hold the center button until the light turns on. The indicator lights on the device will be green if everything is connected correctly. A red light means that an accessory needs to be adjusted or reattached.
Step 8:
Sleep as you normally would. When you wake up in the morning, press the center button for three seconds to stop the test. A green light indicates that the test is complete. A red light indicates that there was an error, and you should talk to your doctor about repeating the test.
Sleep Data Results and Diagnosis
Since the ApneaLink Air records data on the device itself, users do not need a smartphone connection to operate the test. However, this also means that the device needs to be returned in order for the data to be reviewed.
How long it takes to receive your results will depend on your doctor, and it may be worth asking about the post-test diagnosis process and timeline before using the test. Some medical professionals may call you with the results, while others may require an in-office visit followup.
Use this SleepApnea.org link for the most current discount on ResMed products
Shop NowWhat Do Customers Have to Say About the ApneaLink Air?
Most people discussing the ApneaLink Air online report positive experiences.
The test’s signal indicators received particular praise, as they allowed many users to feel confident that they set the test up correctly. Users also liked the test’s streamlined design, which they felt provided their doctors with accurate information while still making it easy to sleep.
However, some users still felt that the test was uncomfortable enough to make sleep challenging. Some people also found the setup confusing, particularly if their doctor did not walk them through the process before giving them the test to take home.
Warranty and Shipping Policies
| Availability | The ApneaLink Air is usually provided by a health care professional. ResMed does not sell the test to the general public. |
| Shipping | Your doctor will explain their return policies when they rent you the device. The ApneaLink Air must be returned to your doctor in order for them to access your data and provide a diagnosis. |
| Warranty | ResMed backs its portable diagnostic devices, including the ApneaLink Air, with a two-year warranty against material or manufacturing defects. |
Medical Disclaimer: This content is for informational purposes and does not constitute medical advice. Please consult a health care provider prior to starting a new treatment or making changes to your treatment plan.
Still have questions?
Sleep apnea products can be confusing. If you need individualized assistance, send us an email at [email protected] with your questions and we'll help find the best fit for you.