As many as 70 million people in the United States have a sleep disorder. Sleep disorders interfere with normal sleep and can negatively affect both your health and quality of life. A sleep study, also called polysomnography, can help find the cause of sleep problems.
Sleep studies can help diagnose sleep apnea and other disorders, help to optimize treatment for sleep apnea, and check whether that treatment is effective. Learn more about sleep studies, including how sleep studies work, the different types of sleep studies, and when to talk to your doctor about whether a sleep study is right for you.
Think You May Have Sleep Apnea? Try an At-Home Test

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
What Is a Sleep Study?
A sleep study, also known as polysomnography, is a medical test that helps doctors evaluate how well you sleep and identify potential sleep disorders. During a sleep study, sensors monitor and record key body functions to give a detailed picture of what happens while you sleep. These measurements include:
- Brain waves
- Eye movements
- Blood oxygen levels
- Heart rate and rhythm
- Breathing patterns and airflow
- Snoring
- Body movements
- Sleeping position
How Does a Sleep Study Work?
Sleep studies are most often performed overnight in a hospital or accredited sleep center, where the testing environment is designed to feel as comfortable as possible, often resembling a bedroom rather than a medical facility. In some cases, doctors may recommend an at-home sleep study, which uses portable equipment to record your breathing and oxygen levels while you sleep in your own bed.
During an in-lab sleep study, the room is equipped with a camera and two-way audio system, allowing you to communicate with the sleep technician if needed. Before the test begins, a trained sleep technologist will help you get settled and attach sensors that record important data while you sleep. These sensors (electrodes) are placed on your scalp, chest, legs, and near your nose and mouth to monitor your brain activity, heart rate, breathing, movement, and oxygen levels.
You may be asked to avoid caffeine or alcohol on the day of the study, since they can affect sleep quality. Many people bring their own pajamas, pillow, or other comfort items to help them relax. Once everything is in place, the lights are turned off, and you’re encouraged to fall asleep as you normally would. A sleep technician remains available all night to assist you if needed. In the morning, the sensors are removed, and your results are analyzed by a sleep specialist to determine whether any sleep disorders are present.
How Long Is a Sleep Study?
Most overnight sleep studies last about six to eight hours, depending on when you fall asleep and wake up. You’ll typically arrive at the sleep center in the evening and leave early the next morning. This allows enough time for specialists to record a full night of data, including several sleep cycles.
Home sleep studies are usually shorter and focus on measuring breathing and oxygen levels over one night. In some cases, your doctor may ask you to repeat a home study for additional accuracy.
What Can a Sleep Study Diagnose?
Polysomnography provides a wide variety of measurements that can help your doctor evaluate sleep problems. Measurements are recorded by a computer system and then evaluated by the sleep technician to look for any signs of sleep issues.
After the sleep study is complete, your results will be forwarded to your doctor or sleep specialist, who will contact you to share the results as well as treatment options. Polysomnography can be used to diagnose a variety of sleep disorders.
- Sleep apnea: Sleep apnea causes repeated interruptions in nighttime breathing. A sleep study can confirm a diagnosis and the degree of sleep apnea, find the right settings for a CPAP machine, and confirm that treatments are effective.
- Sleep-related breathing disorders: In addition to sleep apnea, polysomnography can identify other types of sleep-related breathing disorders.
- Insomnia: Insomnia interferes with the quality and quantity of sleep, such as falling asleep and staying asleep. While most people with insomnia don’t need a sleep study, this testing may be recommended if the causes of insomnia aren’t clear from your medical history and a physical exam.
- Narcolepsy: Narcolepsy inhibits the body’s ability to properly regulate sleep. Polysomnography may be used in combination with other examinations to diagnose narcolepsy.
- Hypersomnia: Hypersomnia describes excessive tiredness that isn’t improved by sleep or napping. Polysomnography can help find the cause of these symptoms and can diagnose idiopathic hypersomnia, a type of hypersomnia in which the cause is unknown.
How Do You Get a Sleep Study?
If you’re struggling with unrefreshing sleep or ongoing fatigue, you don’t have to simply live with it. A sleep study can help uncover what’s causing your symptoms and guide you toward effective treatment. Talk to your doctor if you or a loved one notice any of the following signs:
- Difficulty falling or staying asleep
- Excessive daytime sleepiness or dozing off unexpectedly
- Loud, frequent snoring or gasping for air during sleep
- Waking up feeling short of breath
- Uncomfortable sensations or restlessness in your legs
- Unusual movements or behaviors while asleep
Your doctor will start by asking about your sleep habits, medical history, and symptoms. They may also perform a physical exam to look for signs of sleep-related breathing issues or other disorders. Based on what they find, your doctor might suggest lifestyle changes, recommend an at-home sleep test, or refer you to a sleep specialist for a more detailed evaluation in a sleep center.
How Much Does a Sleep Study Cost?
The cost of a sleep study depends on your health insurance coverage. If you have health insurance, contact your provider for information about your plan’s deductible, copayments or coinsurance, and your out-of-pocket maximum. Medicare and many other insurance plans only provide coverage for sleep studies under certain circumstances.
If you don’t have health insurance, talk to your doctor and the billing or financial department at the location where you receive care. Your doctor or the facility conducting the sleep study may have information about discounted services, financial assistance, or help enrolling in a health care plan.
What Are the Other Types of Sleep Studies?
While in-lab polysomnography is the gold standard type of sleep study to diagnose obstructive sleep apnea (OSA), there are several other types of sleep studies that may be used in select circumstances. Your doctor or a sleep specialist will determine the best type of sleep study based on your individual needs.
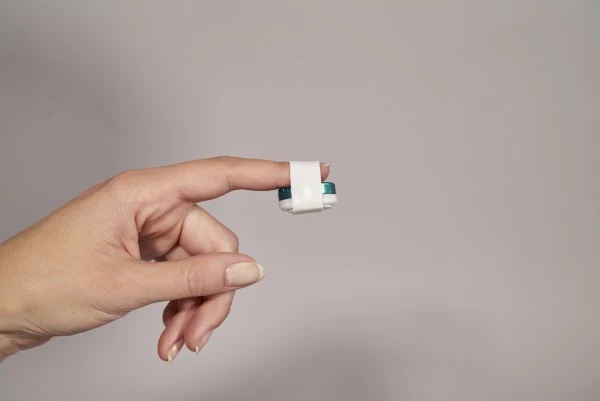
At-Home Sleep Study
An at-home sleep study is a convenient alternative to testing in a hospital or sleep lab. Doctors often recommend it when obstructive sleep apnea (OSA) is strongly suspected. Home tests use portable equipment to measure breathing patterns, oxygen levels, and heart rate while you sleep in your own bed.
Before testing, a provider will explain how to place the sensors and operate the device. Once the study is complete, your doctor reviews the recorded data to determine whether OSA is present or if your current CPAP therapy is working effectively.
While home sleep tests are comfortable and accessible, they collect fewer data points than in-lab polysomnography and don’t include real-time monitoring by a technician. They are best suited for people with moderate to severe OSA and are not recommended if:
- Your doctor suspects that you have another type of sleep disorder, including central sleep apnea.
- You have another medical condition contributing to your nighttime breathing issues.
- You're a pilot, driver, first responder, member of the military, or work in another role where daytime alertness is essential for safety.
- You’ve already tried an at-home sleep apnea test and had negative or inconclusive results.
Children's Sleep Study
A children’s sleep study (pediatric polysomnography) is used to diagnose sleep disorders in infants, children, and adolescents. It measures breathing, brain activity, oxygen levels, and body movements while your child sleeps in a comfortable, supervised setting.
Doctors may recommend a children’s sleep study if your child snores frequently, has pauses in breathing, or shows signs of excessive daytime sleepiness, hyperactivity, or behavioral changes. The results help identify conditions such as obstructive sleep apnea, nighttime seizures, or movement disorders, so your child can receive appropriate treatment.
CPAP Titration Sleep Study
A CPAP titration sleep study is performed after a diagnosis of obstructive sleep apnea to determine the most effective air pressure settings for continuous positive airway pressure (CPAP) therapy.
During this study, a technician monitors your sleep while gradually adjusting CPAP pressure levels to find the setting that keeps your airway open and minimizes breathing interruptions. This ensures that your treatment is both comfortable and effective, helping you achieve deeper, more restorative sleep.
Multiple Sleep Latency Test
A multiple sleep latency test (MSLT) measures how quickly you fall asleep during the day and how soon you enter rapid eye movement (REM) sleep. Doctors use it to help diagnose or rule out narcolepsy, idiopathic hypersomnia, and other causes of excessive daytime sleepiness.
The MSLT typically takes place the day after an overnight sleep study. You’ll take five scheduled naps, each lasting about 20 minutes and separated by two-hour breaks during which you stay awake. Results show how easily you fall asleep in quiet conditions, providing valuable information about your daytime alertness and sleep regulation.
Maintenance of Wakefulness Test
A maintenance of wakefulness test (MWT) measures how well you can stay awake during the day. Doctors often use it to evaluate daytime alertness or to see whether sleep apnea treatment or other therapies are working effectively.
The MWT usually begins a few hours after waking and includes four testing periods, each up to 40 minutes long, with two-hour breaks between sessions. You’ll sit in a quiet, dimly lit room and be asked to remain awake for as long as possible while your brain activity and eye movements are monitored.
Actigraphy
Actigraphy is a noninvasive way to monitor your sleep-wake patterns over days or weeks using a wrist-worn activity tracker. The device measures movement, rest periods, and light exposure to estimate when you’re asleep or awake.
Doctors may recommend actigraphy to track sleep schedules, insomnia patterns, or treatment progress. While many consumer devices measure sleep, medical-grade actigraphy provides more reliable data. These devices are simple to use, rechargeable, and often prescribed for long-term sleep monitoring.
Frequently Asked Questions
It’s common to worry about falling asleep during a sleep study, especially in a new environment. Fortunately, technicians only need a few hours of recorded sleep to get accurate results. Most people sleep enough for the test to be valid, even if they feel like they barely slept. If you have ongoing difficulty, your doctor may discuss mild sleep aids or schedule another study to ensure accurate results.
Many health insurance plans, including Medicare, cover at-home sleep studies when they’re ordered by a doctor to test for obstructive sleep apnea. Coverage may vary depending on your plan and provider, so it’s best to confirm eligibility and any out-of-pocket costs before scheduling the test. Your sleep specialist or testing provider can help you verify coverage and submit the necessary documentation.
In most cases, no, a prescription is required for a CPAP machine in the U.S. This ensures that your pressure settings are accurate and that therapy is safe and effective. A sleep study (either at-home or in-lab) is needed to confirm a diagnosis of sleep apnea and determine the correct treatment plan. Buying or using a CPAP device without a prescription can lead to improper pressure levels and ineffective therapy.
Policies vary by sleep center, but most adult sleep studies are conducted alone to avoid distractions and ensure accurate results. However, exceptions are often made for children, people with disabilities, or those who need assistance during the night. If you feel anxious about the study, let your sleep center know. Technicians can explain the process, provide reassurance, and help you feel more comfortable throughout the night.
In a full-night sleep study, polysomnography is only used to assess sleep health and test for sleep apnea. If the test shows that you have sleep apnea, you may be asked to schedule an additional overnight visit to the sleep clinic for CPAP titration. In a split-night study, the first half of the night is used to diagnose sleep apnea, and the second half is used for CPAP titration.