At a Glance:
- 66.7% of U.S. adults with obstructive or central sleep apnea found out they had it after taking an at-home test, according to a survey.
- 59.1% found out after explaining symptoms to their physician.
- 55% of adults diagnosed with obstructive sleep apnea say they've snored in the past five years.
- 76.7% of adults consider untreated sleep apnea a serious health risk.
- 40.3% of people diagnosed with sleep apnea have not tried any treatment.
A nudge from his wife led Joe Karasin to see his primary-care physician.
“She was bothered by my snoring and the fact that I would stop breathing in the middle of the night,” he says.
Karasin, 38, of Chicago, says his doctor referred him to a sleep center that gave him an at-home test. A home sleep study test (HST) typically includes a monitoring device with sensors that measure body metrics such as respiratory effort, heart rate, blood oxygen, and snoring. After the results came back, a physician diagnosed Karasin with obstructive sleep apnea (OSA).
How do people find out they have sleep apnea? Many are just like Karasin, as two-thirds (66.7%) of U.S. adults diagnosed with obstructive or central sleep apnea (CSA) first find out via an at-home test, according to an April 2023 SleepApnea.org survey. These tests have grown in popularity, supplementing or replacing the traditional polysomnography (PSG) sleep study in a laboratory or physician's office. Many treatments such as continuous positive airway pressure (CPAP) therapy, however, require a prescription that comes after a physician's diagnosis.
Meanwhile, 47% of adults with sleep apnea say they first found out after someone else pointed out their snoring, with 43.2% turning to an HST after that.
“Most people don’t know they have sleep apnea, and the majority of my patients are brought in by a spouse or parent who overheard them snoring,” says Dr. Jag Sunderram, professor of medicine and interim chief of the Division of Pulmonary and Critical Care Medicine at Rutgers University’s Robert Wood Johnson Medical School. “Sleep disorders and sleep apnea are a growing concern.”
About 20% of U.S. adults have OSA, but about 90% go undiagnosed1. Understanding the symptoms for OSA and CSA and how diagnosis occurs for most folks can help in addressing sleep apnea quickly and mitigating the health risks.
When It's More Than Just Snoring
Snoring is the top symptom reported among folks with OSA, which occurs when the upper airway partly or fully collapses and makes breathing difficult. Exactly 55% of survey respondents with OSA reported snoring in the past five years, a percentage that jumped to 74.1% of adults whose diagnosis came from a physician.
With CSA, however, the brain fails to signal the muscles that control breathing. That could help explain why fatigue is cited as the No. 1 symptom among all respondents diagnosed with CSA (62.5%), though 73.7% of adults with physician-diagnosed CSA say they've snored in the past five years.

How do we know when our snoring indicates something more serious? Typically other symptoms accompany snoring. Other top symptoms for all respondents diagnosed with sleep apnea show how the disorder can impact our sleep, daytime functioning, and overall health. They include the following:
- Insomnia: 31.5%
- Daytime sleepiness: 35.5%
- Difficulty focusing or concentrating: 30.6%
- Morning headaches: 28.2%
- High blood pressure: 21%
Having any of these symptoms doesn't mean you have sleep apnea, as they can also occur with other sleep disorders2. Statistics on the amount of U.S. adults with OSA or CSA vary. According to the survey, 5.3% of U.S. adults have a sleep apnea, with OSA skewing 55% male and CSA 58.3% male.
Although at-home tests were the most popular way respondents discovered their sleep apnea, 59.1% say their physician suggested it, and 57.6% of adults with sleep apnea saying they received a diagnosis after bringing up the symptoms with a physician.
“Sleep apnea is serious and can be treated,” says Dr. Joseph Krainin, SleepApnea.org's medical advisor.
Talking Sleep With Your Doctor
In addition or in place of symptoms, risk factors may provide clues about sleep apnea. Studies show people who are ages 65 or older, male, and have facial features such as a short lower jaw or a wide facial shape are more likely to have sleep apnea3.
“Another indicator of sleep apnea is obesity,” Dr. Krainin says. “However, you can’t look at someone’s BMI [body mass index] and tell if they have sleep apnea. Someone who’s overweight may not have it, and someone who’s thin can have it.
“If you suspect you have sleep apnea or if you are constantly fatigued after you believe you had a full seven or eight hours of sleep, talk to your doctor.”
Often, however, sleep apnea may not come up in a typical doctor visit, hence the popularity of at-home sleep studies. That's because many primary care physicians receive minimal training in sleep medicine4, Dr. Sunderram says.
“Annual wellness exams take less than an hour, and a lot is covered in that time,” he says. “Unless a physician notices a fatigued patient, it’s not discussed.”
JaneA Kelley, 54, of Washington state says didn’t take her snoring seriously until a friend heard her gasping for air during the night. That led her to book a doctor appointment and receiving an OSA diagnosis.
“It had always been a running joke in my family,” Kelley says, “but nobody ever thought this might be something that required medical attention.”
Understanding the Risks of Undiagnosed Sleep Apnea
Untreated sleep apnea can have serious health consequences5, such as a higher risk of high blood pressure, diabetes, and having a stroke.
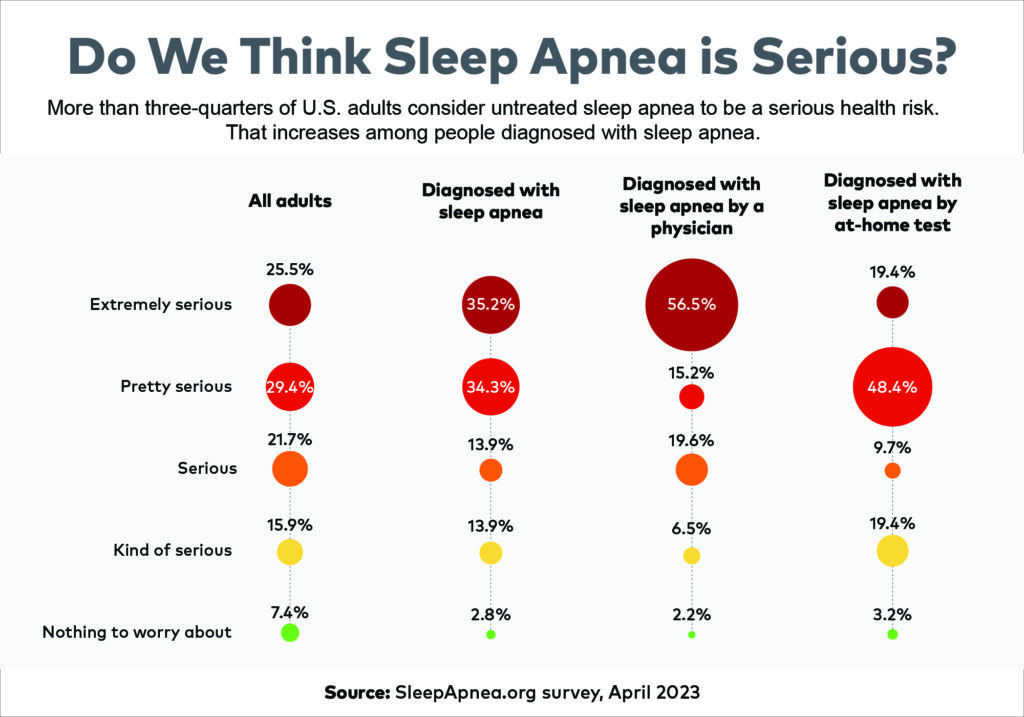
Understanding sleep apnea may contribute to understanding its risks. Among all survey respondents, 76.7% say sleep apnea is a serious health risk. Those diagnosed with sleep apnea are 8.6% more likely to consider it serious than those who haven’t been diagnosed. Talking with a physician may drive the point home: 91.3% of those diagnosed by a physician understand sleep apnea is a health risk if left untreated. That's 19% more than average and 18% more than those who find out via an HST.
But understanding the health risk doesn’t always mean folks seek the treatment they need for sleep apnea. Some 40.3% of adults who have received a sleep apnea diagnosis have not tried any treatment.
CPAP therapy, which uses a device with compressed air to help open airways during sleep, is the most common treatment. While it’s not the only treatment for sleep apnea, it’s the gold standard, Dr. Krainin says.
Survey respondents who have had symptoms in the past five years have seen some resolve since using a CPAP or BiPAP machine. BiPAP machines release two levels of airway pressure instead of one, commonly used for CSA. More than half of respondents say their snoring got better (61.9%), their insomnia improved (58.8%), and they are less fatigued (58.3%) after using a CPAP or BiPAP machine.
Kelley uses a nasal pillow CPAP mask, an option that is easier for some, including side sleepers or those with claustrophobia.
“It was a little strange at first, and then I became comfortable with it after a couple of days,” she says. “I wake up refreshed.”
Methodology
The survey commissioned by SleepApnea.org was conducted on the online survey platform Pollfish on April 5, 2023. Results are from 1,250 survey participants in the United States who were age 18 or older at the time of the survey. All respondents attested to answering the survey questions truthfully and accurately.








