At a Glance
Diagnosing sleep apnea usually begins with a review of symptoms, medical history, and risk factors such as loud snoring, daytime sleepiness, or breathing pauses during sleep. A doctor typically confirms the diagnosis with a sleep study — either in a lab or at home — which measures breathing patterns and calculates an apnea-hypopnea index (AHI) to determine severity.
A growing number of people in the United States are being diagnosed with sleep apnea, a disorder characterized by repeated pauses in breathing, most often due to airway obstruction. These breathing interruptions can have serious consequences stemming from drops in blood oxygen levels and disrupted sleep.
Sleep apnea can be effectively managed in a number of ways. But in order to plan treatment, an accurate diagnosis must be made. Learning about the diagnostic process for sleep apnea can help you have an informed discussion with your doctor about your symptoms and next steps for care.
Think You May Have Sleep Apnea? Try an At-Home Test

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
Initial Signs and Symptoms
The first step in figuring out if you have sleep apnea is recognizing the symptoms. Sleep apnea may present itself in a number of ways. Consider talking with your doctor if you have one or more of these common sleep apnea symptoms.
- Loud snoring or gasping for air during sleep: A partner or a family member may notice that you are snoring or experiencing shallow or irregular breathing.
- Daytime sleepiness: Daytime sleepiness includes feelings of low energy or poor focus. People with sleep apnea may also unintentionally fall asleep during daytime activities.
- Morning headaches: Morning headaches that occur daily or multiple times a week are reported by some people with obstructive sleep apnea.
- Sleep-maintenance insomnia: Waking up multiple times in the night can be a symptom of sleep apnea. Repeated awakenings may lead to more urges to urinate in the night.
Medical History and Physical Exam
In order to determine whether you should be referred for a sleep study, a doctor will first perform a physical exam, ask about symptoms, and collect your personal and family history. During an evaluation for sleep apnea, a doctor may ask one or more of the following questions:
- Do you feel tired or sleepy during the day?
- Has anyone told you that you snore loudly or have pauses in breathing during your sleep?
- Is it difficult to stay awake performing tasks like driving, reading, or watching TV?
- Do you currently smoke, or have you smoked in the past?
- Has anyone in your family been diagnosed with sleep apnea?
Risk Factors for Sleep Apnea
During the exam, the doctor may also take into consideration the following factors, which put you at higher risk of sleep apnea.
- Large neck circumference: A neck with a circumference greater than 17 inches for men and 15.5 inches for women may indicate excess fat, including tongue fat, that could narrow or block the airway.
- Age: Individuals older than 65 are at higher risk for central sleep apnea.
- Misaligned jaw: A small lower jaw or an abnormally shaped upper jaw may impact positioning of the tongue, which in turn can block the airway during sleep.
- Family history of snoring and apnea: The risk of developing obstructive sleep apnea is approximately 50% greater if a first-degree relative such as a sibling or parent has the condition.
- Cardiovascular issues: People with cardiac conditions, including high blood pressure and heart failure, commonly have sleep apnea.
Sleep Diary
Your doctor may ask you to keep a sleep diary for one to two weeks. This record helps capture patterns in your sleep habits, such as when you go to bed, how often you wake up during the night, whether you experience gasping or choking, and how rested you feel in the morning. Tracking factors like caffeine or alcohol consumption, exercise, and use of electronics before bed can also provide valuable context.
While a sleep diary can't diagnose sleep apnea on its own, it offers doctors a clearer picture of your symptoms and lifestyle, which can help guide decisions about whether further testing—like a sleep study—is necessary.
Sleep Study
If the doctor suspects sleep apnea based on your exam and symptoms, they will likely recommend a polysomnogram. This is a sleep study in which medical sensors are used to monitor a person’s breathing, heart rate, and the electrical activity of their brain waves while they sleep. While historically these were conducted in a sleep lab, there are now at-home testing options.
In-Lab Polysomnogram
If you have a polysomnogram at a sleep lab, your health care provider will give you instructions on when to arrive, what to bring with you, and whether you should make any changes to your diet or medications that day.
After acclimating to your room at a sleep lab, a technician attaches monitoring sensors to your legs, fingers, chest, and head. The sensors measure body processes while you sleep. The data are then translated into stages of sleep, wakefulness, and events where breathing is interrupted.
If the doctor thinks it’s very likely that you have sleep apnea, they may order a sleep study with the potential to trial a positive air pressure (PAP) device. This is called a split-night sleep study. If the polysomnogram results from the first half of the night confirm that you have significant sleep apnea, a PAP device will be applied and customized in the second half of the night to help prepare you for ongoing treatment.
A PAP device helps keep the soft tissues of the airway open by routing pressurized and humidified air through a tube and mask fitted to your face while you sleep. Your physiological activity is monitored at different air pressures provided by the PAP device to see which is the best pressure for you.
A polysomnogram at a sleep center may be preferred over a home sleep apnea test if you have heart or lung disease, risk factors for central sleep apnea, or potential to be diagnosed with other sleep disorders.
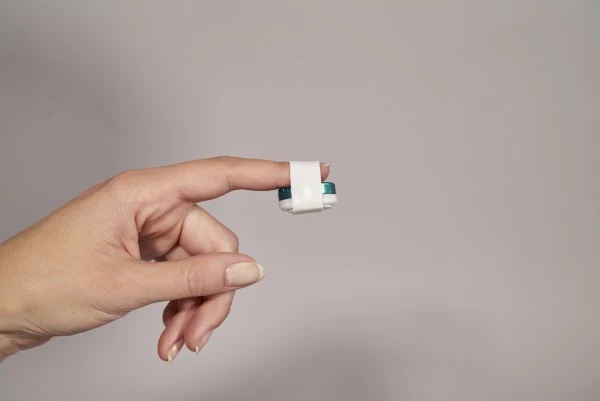
Home Sleep Apnea Tests
A home sleep apnea test (HSAT) may be an option for people who are suspected of having moderate to severe obstructive sleep apnea based on their symptoms, medical history, and physical exam. An HSAT takes fewer measurements than an in-lab sleep study, and does not have brain sensors (EEG) and muscle sensors (EMG) that measure sleep or sleep stages.
That said, home sleep apnea tests do provide some benefits. For example, when a person sleeps in the comfort of their own home, they are more likely to have longer periods of sleep. An HSAT can also be used to help determine whether a PAP device is working well or to reevaluate a person if they are still experiencing symptoms after starting treatment.
Different home sleep apnea test kits are available and your sleep doctor will instruct you on the proper application of the sensors.
After you take a test, your doctor reviews the data and works with you to provide the best course of treatment.
Review Sleep Study Results
Once a sleep study is complete—whether conducted in a lab (polysomnography) or at home—your healthcare provider will review the data to determine whether you have sleep apnea, how severe it is, and what type you may be experiencing.
Diagnostic Criteria
A diagnosis of obstructive sleep apnea is based on the results of the polysomnogram and the presence or absence of certain symptoms. A polysomnogram records how many apneas, hypopneas, or respiratory effort-related arousals (RERA) occur per hour while a person is asleep.
- Apnea: Apnea is when airflow stops for a period of 10 seconds or longer.
- Hypopnea: Hypopnea is a period of shallow breathing that lasts for at least 10 seconds and causes a drop in the oxygen level in your blood or a brief arousal from sleep.
- Respiratory effort-related arousal (RERA): RERAs occur when breathing is restricted more subtly than a hypopnea but is still associated with a brief arousal from sleep.
Apnea-Hypopnea Index (AHI)
The apnea-hypopnea index (AHI) measures the average number of times per hour that your breathing is either partially (hypopnea) or completely (apnea) blocked during sleep. This index is a central metric used in diagnosing sleep apnea. It's calculated by dividing the total number of apneas and hypopneas by the number of hours slept.
The AHI can vary from night to night, but it offers a crucial snapshot of how often breathing disruptions are occurring and how significantly they may be impacting sleep quality and oxygen levels.
Severity Levels of Sleep Apnea
Sleep apnea is categorized based on your AHI score:
- Mild sleep apnea: AHI of 5 to 14 events per hour
- Moderate sleep apnea: AHI of 15 to 29 events per hour
- Severe sleep apnea: AHI of 30 or more events per hour
These classifications help guide treatment decisions. For example, someone with mild sleep apnea might benefit from lifestyle changes or positional therapy, while moderate to severe cases may require continuous positive airway pressure (CPAP) therapy or other interventions.
In addition to AHI, your provider will consider other factors from the sleep study—such as oxygen saturation, sleep architecture, and arousal frequency—to form a complete diagnosis and personalized treatment plan.
Types of Sleep Apnea
Your sleep study will also identify the type of sleep apnea you have, which influences the recommended treatment approach:
- Obstructive Sleep Apnea (OSA): The most common type, OSA is caused by a physical blockage of the airway, usually due to relaxed throat muscles or tissue collapse.
- Central Sleep Apnea (CSA): In CSA, the brain doesn’t send consistent signals to the muscles that control breathing, leading to pauses in breath without any physical obstruction.
- Complex or Mixed Sleep Apnea: This is a combination of obstructive and central events. It sometimes emerges after starting CPAP therapy for OSA and requires specialized treatment.
Next Steps After Diagnosis
If you're diagnosed with sleep apnea, a member of your healthcare team will explain what type of sleep apnea you have and whether the condition is mild, moderate, or severe. They may also talk about some of the potential health risks associated with sleep apnea and offer precautions against driving if you are frequently sleepy during the day.
Next, a doctor will discuss what kind of treatment is appropriate for your situation. Your treatment for sleep apnea will depend upon what type of sleep apnea you have and the severity of the disorder, as well as your personal preferences.
For most people, sleep apnea is a chronic condition. This means that ongoing treatment usually alleviates symptoms, but stopping treatment will cause the condition to come back. Over time, it is common for sleep apnea to slowly get worse.
For most people, sleep apnea can be managed effectively with a combination of medical treatment and healthy sleep habits.
- Positive airway pressure therapy: PAP therapy is a primary treatment option for OSA and certain types of CSA. A PAP device has a mask that is worn over your nose and mouth during sleep. The mask is connected by a hose to a small machine beside your bed, and the machine pumps air through the hose and mask to open your airway.
- Oral appliances: Apart from PAP, there are also oral appliances that position your tongue or jaw in a way that doesn’t block airflow. These oral appliances may be considered for some people as an alternative treatment to PAP therapy.
- Healthy sleep habits: Regular physical activity, losing weight, and maintaining healthy sleep habits may relieve symptoms of sleep apnea. Changing your sleep position from sleeping on your back to sleeping on your side may also help.
- Surgery: Surgical treatment may be an option for some people. The goal of surgery is to stabilize or enlarge the upper airway in order to improve airflow. It is hard to predict who will respond well to a surgical procedure, and it is common for residual OSA to persist. In this case, the surgery may make PAP therapy more tolerable and effective.
- Nerve stimulation: Another option for people who are not able to tolerate PAP therapy is a surgically implanted device in the upper chest. This device connects to a nerve that pushes the tongue forward with breathing in order to help clear the airway. Multiple criteria must be satisfied to pursue this type of treatment for obstructive sleep apnea.
Frequently Asked Questions
While a sleep study is the gold standard for diagnosing sleep apnea, a healthcare provider may suspect sleep apnea based on your symptoms, medical history, and physical exam. However, a formal diagnosis requires objective evidence of disordered breathing during sleep—something only a sleep study (either in-lab or at-home) can provide.
In some cases, a doctor may begin treatment based on strong clinical suspicion, but a sleep study is typically needed to confirm the diagnosis and determine severity.
Several conditions share similar symptoms with sleep apnea, including chronic insomnia, upper airway resistance syndrome (UARS), restless legs syndrome (RLS), depression or anxiety, chronic fatigue syndrome, or heart failure or other cardiopulmonary disorders.
These conditions can cause fatigue, unrefreshing sleep, and even nighttime awakenings, making them easy to confuse with sleep apnea. A sleep study helps distinguish between these conditions by monitoring your breathing patterns during sleep.
No, blood work cannot directly diagnose sleep apnea. Sleep apnea is a mechanical and neurological breathing disorder, diagnosed through observation of breathing disruptions during sleep.
However, blood tests may help identify related issues such as low oxygen levels, elevated carbon dioxide, or conditions that can contribute to or result from sleep apnea (like hypothyroidism or high red blood cell counts). Blood work can be a useful part of the overall diagnostic process, but it can’t confirm or rule out sleep apnea on its own.