If you’ve been told that you stop breathing while you sleep, snore loudly, or wake up gasping for air at night, you may wonder if you have sleep apnea. Sleep apnea is a common condition that affects nearly 30 million people in the U.S. Without treatment, sleep apnea can interfere with quality sleep and increase your risk of health complications.
Fortunately, treatment for sleep apnea can help you sleep better, restore healthy breathing, and decrease the risk of long-term health issues. If you’re concerned you may have sleep apnea, it’s important to learn more about the condition and contact your doctor. They can evaluate your symptoms and, if necessary, order a sleep study to confirm their diagnosis.
Think You May Have Sleep Apnea? Try an At-Home Test

our partner at sleepdoctor.com
10% off Home Sleep Tests
Buy Now“Truly grateful for this home sleep test. Fair pricing and improved my sleep!”
Dawn G. – Verified Tester
What Is Sleep Apnea?
Sleep apnea is a common sleep disorder that affects nighttime breathing. After a person with sleep apnea dozes off, they begin to alternate between periods of normal breathing and episodes when their breathing becomes shallow or stops completely.
These repetitive breathing disruptions cause changes in the body that, without treatment, can reduce sleep quality, contribute to sleepiness the following day, and increase the risk of long-term health issues.
There are two forms of sleep apnea, obstructive sleep apnea and central sleep apnea.
Obstructive Sleep Apnea
Most people with sleep apnea have obstructive sleep apnea. In obstructive sleep apnea, nighttime breathing issues are caused by a blockage in the airway. Blockages can develop in one or more places in the upper airway, including inside the nose, at the back of the tongue, and as far down as the voicebox.
Central Sleep Apnea
Central sleep apnea is a less common form of sleep apnea. When a person has this type of sleep apnea, their airway remains open during sleep. Instead, lapses in breathing occur because the brain temporarily stops telling the body when to breathe. Central sleep apnea is usually caused by an underlying health condition or is the side effect of a medication.
How Sleep Apnea Is Diagnosed
Diagnosing sleep apnea starts with an evaluation by a doctor or sleep specialist, who will review your symptoms, medical history, and risk factors. They may ask about snoring, nighttime awakenings, gasping or choking sounds during sleep, and how rested you feel during the day. Because people often don’t notice their own nighttime symptoms, a bed partner’s observations can be especially helpful.
Symptoms of Sleep Apnea
The symptoms of sleep apnea depend on the severity and underlying cause of breathing issues. Everyone with sleep apnea experiences irregular breathing after falling asleep, but many don’t notice other common symptoms or mistakenly believe that their symptoms are a normal part of getting older.
- Snoring: People with sleep apnea may snore, snort, choke, or gasp during periods of irregular breathing at night. Almost everyone with sleep apnea snores, though not all people who snore have sleep apnea.
- Daytime sleepiness: Frequent nighttime awakenings can contribute to feeling excessively tired during the day. Tiredness may persist throughout the day or get worse while driving, watching television, or while engaging in other passive activities.
Additional symptoms of sleep apnea include:
- Daytime headaches
- Dry mouth
- Difficulty with concentration and memory
- Nighttime chest pain
- Getting up at night to use the bathroom
Because the most recognizable symptoms of sleep apnea begin during sleep, people may not be aware of their symptoms until a roommate or bed partner mentions them.
Sleep Study
A physical exam may also be performed to look for features that increase sleep apnea risk, such as a narrowed airway, enlarged tonsils, or a higher body mass index (BMI). If sleep apnea is suspected, the next step is a sleep study, which provides the data needed for a formal diagnosis.
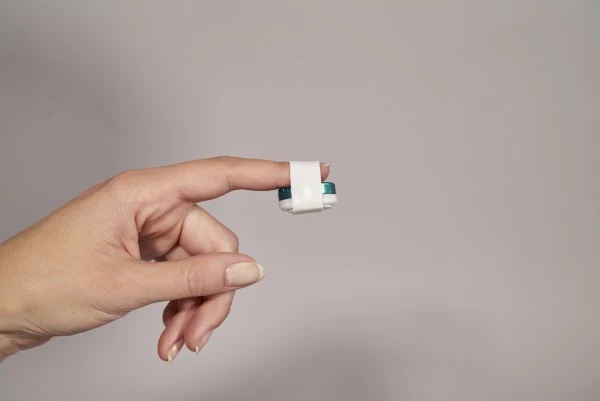
Sleep apnea can be confirmed through either an overnight sleep study in a sleep lab—called polysomnography—or an at-home sleep apnea test. A lab study can detect all types of sleep apnea and tracks a wide range of measurements, including brain waves, airflow, breathing effort, oxygen levels, heart rate, and sleep stages. At-home sleep apnea tests are simpler and typically recommended for people with symptoms of moderate to severe obstructive sleep apnea. They measure breathing patterns, airflow, and oxygen levels while you sleep in your own bed.
Sleep Apnea Diagnosis
A sleep specialist will review the results of your study to determine whether you have sleep apnea, what type you have, and how severe it is. Diagnosis is based in part on your apnea-hypopnea index (AHI), which reflects how many breathing pauses or shallow breaths you experience per hour of sleep.
- Mild sleep apnea: an AHI of 5 to 14
- Moderate sleep apnea: an AHI of 15 to 29
- Severe sleep apnea: an AHI of 30 or more
These findings help guide your treatment plan and determine the most appropriate therapy for your needs.
Causes of Sleep Apnea
The cause of obstructive sleep apnea is an obstruction in the airway. The cause of central sleep apnea is a lack of communication between the brain and the respiratory muscles, often related to another health condition like heart failure or stroke.
Risk Factors for Sleep Apnea
Anyone can have sleep apnea, but certain risk factors increase the likelihood that a person will develop these sleep-related breathing disorders.
- Older age: Getting older increases the risk of both obstructive and central sleep apnea. The risk of obstructive sleep apnea peaks in a person's 60s and 70s, while central sleep apnea is most common in people over 65 years old.
- Male sex: Men and people assigned male at birth are at a heightened risk of both types of sleep apnea. Experts suggest that this increased risk may be related to the effects of hormones on breathing.
- Physical features: Some people are more prone to developing obstructive sleep apnea because of the shape, size, or position of certain physical features. Features that may increase the risk of breathing issues during sleep include a short lower jaw, wide facial shape, or enlarged tissues in the throat.
- Medical conditions: A wide variety of medical conditions increase the risk of sleep apnea. These conditions include heart failure, stroke, high blood pressure, atrial fibrillation, and diseases of the lungs or kidneys.
- Medications and substances: Certain medications, as well as substances like alcohol and opioids, can make a person more likely to develop sleep apnea or make existing sleep apnea worse. Other medications that increase the risk of sleep apnea include some antidepressants and benzodiazepines.
Other potential risk factors for obstructive sleep apnea include smoking, nasal congestion, environmental exposures, and a family history of snoring or obstructive sleep apnea.
In children, the most significant risk factors for obstructive sleep apnea are obesity and enlarged adenoids and tonsils. Enlarged tonsils or adenoids may be due to inflammation, infection, or genetics.
When to Talk to Your Doctor
If you’re experiencing any symptoms of sleep apnea, including loud snoring or unexplained daytime tiredness, it’s important to contact your health care provider. Also talk to your doctor if a roommate or bed partner notices severe snoring or breathing changes as you sleep.
To diagnose sleep apnea, a doctor will ask about your medical history, conduct a physical exam, and recommend tests to understand the cause of your symptoms. The most important test used to diagnose sleep apnea is a sleep study, which is also called polysomnography. A sleep study is a test conducted overnight in a special sleep laboratory or, in some cases, in your home.
Treatment for Sleep Apnea
Treatment for sleep apnea is chosen based on the type of sleep apnea diagnosed and the severity of the condition. As central sleep apnea is most often related to another condition, initial treatment is usually geared towards addressing that underlying medical issue.
In people with obstructive sleep apnea, doctors may recommend certain behavior changes, including caution when operating a vehicle due to the increased risk of sleepiness-related accidents. Doctors may also recommend an exercise or weight-loss program for people who are overweight or have obesity.
People with sleep apnea should also be aware of factors that may worsen their nighttime breathing, such as alcohol or sedating medications. In some cases, obstructive sleep apnea worsens when a person is lying on their back, so doctors may offer advice on changing the position in which they sleep.
Positive Airway Pressure (PAP) Therapy
Continuous positive airway pressure (CPAP) is a treatment that keeps the airway open during sleep by pumping pressurized air through a mask. CPAP is the most commonly prescribed treatment option for people with central or obstructive sleep apnea. To get the most out of CPAP, it’s important to use the device every night.
CPAP is just one type of positive airway pressure device. Other ways of delivering positive airway pressure include auto-adjusting positive airway pressure (APAP), bilevel positive airway pressure (BiPAP or BPAP), and adaptive servo-ventilation (ASV) machines.
Other Treatments
Other treatments for sleep apnea may be recommended based on a person’s individual needs.
- Oral Appliances: Oral appliances may be recommended for some people with obstructive sleep apnea. These devices are worn in the mouth to keep the airway open during sleep. Like CPAP, people must use oral appliances consistently to get the best results.
- Surgery: Surgery to remove the tonsils and adenoids may be the first treatment recommended for children with obstructive sleep apnea. Doctors may also recommend surgery for adults with obstructive sleep apnea when other treatments aren’t working. There are a wide variety of surgeries that may be used to prevent the airway from closing during sleep.
- Medications: Although medications are sometimes used to treat central or obstructive sleep apnea, some medicines are associated with a significant risk of side effects. Medications are usually only used when other treatments aren’t effective.
- Nerve Stimulation: With nerve stimulation, a medical device is implanted in the body to normalize breathing. In obstructive sleep apnea, a nerve stimulation device prevents the airway from collapsing. In central sleep apnea, a different implantable medical device stimulates breathing muscles.
Healthy Sleep Habits
Cultivating healthy sleep habits is important for everyone, but getting enough sleep each night may be particularly important if you’re living with obstructive sleep apnea. Consider implementing some tips that could improve your sleep.
- Stay consistent: Stick to a consistent sleep routine, making sure to give yourself enough time to relax before bed and go to bed at the same time every night. Getting up at the same time every morning can also help get your body into a routine.
- Exercise: Exercise can improve sleep, help with weight maintenance, and reduce the symptoms of obstructive sleep apnea. Experts recommend getting at least 30 minutes of activity most days of the week, but try not to work out within a few hours of bedtime.
- Be cautious with substances: Alcohol, nicotine, and caffeine can all disrupt your sleep, so avoid these substances prior to bedtime. Because certain substances can worsen nighttime breathing problems, check with your doctor about the impact of medications and other substance use.