The apnea-hypopnea index (AHI) describes the number of times a person’s breathing slows or stops during an average hour of sleep. The AHI is one of several measures provided by a sleep study, an overnight test typically conducted in a hospital or sleep clinic or at home.
Sleep studies are used to diagnose sleep disorders. The AHI is particularly useful in diagnosing and determining the severity of obstructive sleep apnea (OSA), a sleep disorder in which the throat repeatedly narrows or closes during sleep, causing problematic breathing disruptions.
If you are one of the nearly 30 million adults in the United States who have OSA, knowing the basics about the AHI—including how it’s calculated and why it can change—can help you understand what your AHI score means for your sleep, your breathing, and your health.
What Is the Apnea-Hypopnea Index?
The AHI is a diagnostic tool that tells you the average number of times your breathing either partially or fully stops per hour of sleep.
Three key pieces of information inform the AHI score.
- Number of apneas: An apnea is a total or near total lapse in breathing, indicated by a reduction in airflow of 90% for at least 10 seconds.
- Number of hypopneas: A hypopnea is a partial reduction in breathing. While there are variations in how sleep labs define hypopneas, they typically last for at least 10 seconds and involve at least a 30% drop in airflow.
- Total sleep time: Total sleep time reflects the amount of time spent in a state of low responsiveness, minimal movement, and limited metabolic activity.
The AHI is calculated by adding the total amount of apneas and hypopneas during the study and dividing that number by total sleep time. This produces a single number that shows how frequently, on average, you experience breathing disruptions during sleep. For example, a person who experiences 15 apneas and 27 hypopneas over the course of seven hours of sleep would have an AHI score of 6.
What Do AHI Readings Mean?
After undergoing a sleep study, you and your doctor should receive a report that summarizes the study’s findings. Sleep study reports include tables, graphs, and measurements—including the AHI score—that your doctor can use to make a diagnosis or to inform treatment recommendations.
An AHI score lower than 5 indicates normal, healthy breathing. Occasional reductions in airflow during sleep are not an indication of obstructive sleep apnea, which involves more frequent lapses in breathing.
If your AHI score is between 5 and 14, and you also have identifiable symptoms of OSA, then your doctor is likely to diagnose you with OSA. You may also be diagnosed with OSA if your AHI is 15 or more, whether or not you have any recognizable symptoms of the condition.
If you are diagnosed with OSA, your doctor may classify the condition as mild, moderate, or severe. Although multiple factors are considered in this process, the AHI score serves as a valuable tool in determining the severity of OSA.riods of shallow breathing) occurring, on average, each hour.
| AHI Score in Adults | Severity Level of OSA |
|---|---|
| 5-14 | Mild |
| 15-30 | Moderate |
| 30 or higher | Severe |
Some sleep labs may also divide the AHI score into two different scores—the apnea index (AI) and hypopnea index (HI)—each of which reflects the average hourly incidence of that breathing issue during sleep.
While the AHI can help diagnose and assess obstructive sleep apnea, it cannot do so on its own. Your doctor or a sleep specialist will interpret your AHI score alongside other data from your sleep study, your symptoms, and your health history. This is why it is important to review your sleep study report and to discuss the meaning of your AHI score with a health professional.
Using the AHI With Children
The apnea-hypopneas index is also an important metric for measuring sleep apnea in children. However, the criteria for measuring apneas and hypopneas are different in children than in adults.
Moreover, a different scale is applied to AHI scores to determine the severity of OSA children.
| AHI Score in Children | Severity Level of OSA |
|---|---|
| 1-4.9 | Mild |
| 5-9.9 | Moderate |
| 10 or higher | Severe |
Based on a doctor’s judgment, either the adult or pediatric measurement of AHI may be used for adolescents.
Other Ways to Measure Obstructive Sleep Apnea
The apnea-hypopnea index is just one of several sleep study measurements that health care providers can use to diagnose or determine the severity of sleep apnea. Every approach has benefits and downsides, and it is normal for doctors to consider multiple sources of information when diagnosing and assessing obstructive sleep apnea.
Respiratory Disturbance Index
The respiratory disturbance index (RDI) is another metric that tracks the number of breathing disruptions per hour during sleep. In addition to apneas and hypopneas, the RDI includes respiratory effort-related arousals (RERAs). RERAs involve a reduction in airflow or an increase in breathing effort but aren’t severe enough to be classified as apneas or hypopneas.
Some sleep labs include both the AHI and RDI on their test reports. Because the RDI includes an additional type of breathing disruption, it is always at least as high as the AHI. More research is necessary to determine whether the AHI or RDI is more accurate in diagnosing and assessing the severity of OSA.
Oxygen Levels
The pauses and decreases in airflow that characterize OSA often lead to decreased oxygen levels in the blood. There are a number of metrics related to the amount of oxygen in the blood that sleep studies commonly report.
For example, the oxygen desaturation index (ODI) shows the average number of times per hour that a sleeper experiences an oxygen desaturation, which is a 3-4% drop in blood oxygen levels.
Sleep studies also sometimes measure minimum and average oxygen saturation levels, as well as the amount of time a sleeper spends with below-normal levels of oxygen in their blood—a state known as “hypoxemia.”
Sleep Quality
In addition to documenting breathing disturbances, sleep study technicians also provide information about sleep quality. The breathing problems associated with OSA can cause a person to wake up, leading to fragmented sleep. Additionally breathing disruptions tend to be worse during rapid eye movement (REM) sleep.
As a result, sleep study reports often include information about how often a sleeper wakes up and how much time they spend in different sleep stages.
Is A Sleep Study the Only Way to Get an AHI Score?
It is possible to get an AHI score from some at-home sleep apnea tests. While sleep studies conducted in a laboratory setting are the most thorough and accurate way to assess obstructive sleep apnea, there are a number of portable sleep monitoring devices that can provide useful data from the comfort of your own home.
If you have moderate to severe symptoms of OSA and do not have other medical conditions that affect breathing, your doctor might be able to use data from an at-home test to diagnose OSA. This will allow you to undergo testing in a familiar environment and to generate data over the course of multiple nights, likely at a lower cost than a sleep study.
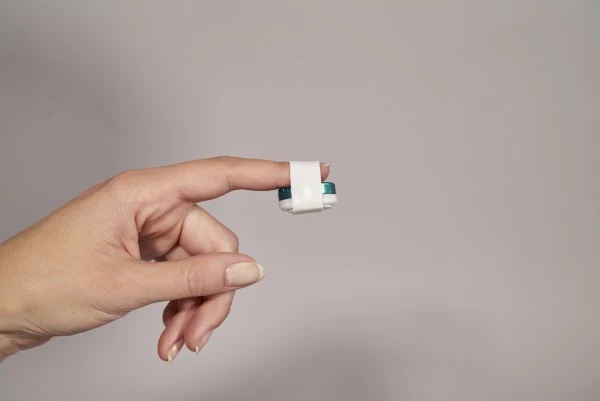
One such device is the “WatchPAT,” which uses a monitor attached to your index finger to record body position, oxygen levels, snoring, heart rate, breathing disturbances, and other data. Following testing, this device generates scores for the AHI, as well as for the respiratory disturbance index and the oxygen desaturation index.
Another option for home AHI testing is to use a specific type of CPAP device called auto-CPAP or APAP. APAP can calculate an estimated AHI based on changes in a person’s airflow while using the device. Though not as precise as the AHI measured during a sleep study, this data may allow your doctor to help you use your CPAP machine more effectively.
It is important to note that at-home tests may not always reliably measure the AHI. A sleep study is the best way to measure breathing disruptions and total time spent sleeping—the key data points used to determine the AHI.
Moreover, because sleep studies assess more variables, they can provide a richer understanding of the relationship between breathing disruptions and other factors, like sleep stages.
Why Does Your AHI Change?
Your AHI score is not a static number. It typically changes throughout the night, as frequency of breathing disruptions can shift based on factors like body position and sleep stage. AHI can also change over a longer period of time—for instance, when treatment for OSA leads to fewer breathing disruptions over the course of a night.
There are multiple reasons why your AHI score can go up or down. However, determining AHI requires careful monitoring during a sleep study or with a validated portable device, so you most likely won’t be aware of short-term increases or decreases in your AHI score.
Causes of AHI Increases
A rising AHI score may be related to one or more factors that are associated with OSA, including:
- Sleeping on your back
- Using alcohol or sedative drugs
- Gaining weight
- Beginning testosterone replacement therapy
If you are concerned that your breathing disruptions at night are getting worse, then you should consult with a medical provider. Your doctor can suggest appropriate testing to assess any potential causes of breathing disruptions.
Causes of AHI Decreases
Many treatments for OSA are designed to reduce your AHI score. Examples of treatments that may reduce AHI scores include:
- Using a CPAP machines, or other type of PAP device
- Making lifestyle changes, such as losing weight or limiting alcohol consumption
- Sleeping on your side instead of your back
- Wearing an oral appliance that repositions the tongue or jaw
- Having surgery to remove tissue that blocks the airway
A doctor or sleep specialist can describe the pros and cons of different OSA treatments and which may work best for you.
Drawbacks of the AHI
The AHI provides a way to quantify breathing disruptions in people with sleep apnea, but it does have drawbacks. Although it is a key tool for doctors and sleep specialists, it must be used as part of a comprehensive evaluation of a person’s symptoms, overall health, and sleep patterns.
AHI Data May Not Be Standardized
While there are criteria for identifying apneas and hypopneas during a sleep study, definitions of these events have changed over the last decade. Because sleep labs may use different definitions of apnea and hypopnea, AHI scores between labs may vary.
AHI Does Not Perfectly Correspond With Symptoms
Although a higher AHI score tends to reflect more severe obstructive sleep apnea, it does not always correspond with a person’s actual symptoms. In some situations, a person can have a high AHI without having any symptoms at all.
AHI and Central Sleep Apnea
In addition to serving as a diagnostic tool for OSA, the apnea-hypopnea index can be used to measure breathing disruptions in central sleep apnea (CSA). The reduced breathing in CSA occurs because of a decrease in the drive to breathe, as opposed to a narrowing or collapse of the airway.
During a sleep study, sensors can detect whether lapses in breathing are likely to be caused by an obstructed airway, a reduced drive to breathe, or a combination of the two. Using this data, separate AHI scores can be calculated for OSA and CSA.