A continuous positive airway pressure (CPAP) machine pumps a steady stream of pressurized air into your airway while you sleep. It is the most common and typically the first recommended treatment for people with sleep apnea, a sleep disorder that affects breathing at night.
CPAP has been shown to improve sleep and to reduce the risk of health issues that untreated sleep apnea can cause. Learning about what a CPAP machine is and how it compares to other sleep apnea treatments can help you make informed decisions about managing your sleep apnea.
What Is a CPAP Machine Used For?
CPAP therapy is used to treat the two main types of sleep apnea: obstructive sleep apnea (OSA) and central sleep apnea (CSA). Both types of sleep apnea cause breathing interruptions during sleep.
CPAP therapy reduces the number of breathing interruptions and snoring severity. In the long-run, CPAP may improve daytime sleepiness and mood and prevent serious health problems.
Doctors typically suggest that people with any severity of OSA try CPAP as a first treatment. But when people with mild to moderate OSA are unable to use CPAP, doctors may give alternative treatment options, like oral appliances.
How Does a CPAP Machine Work?
A CPAP machine works by pumping pressurized air into the airway through a mask. This keeps the airway open and free from blockage to maintain healthy breathing while you’re asleep.
While some CPAP machines provide the same level of air pressure throughout the night, there are other CPAP machines that can automatically change the air pressure based on breathing patterns. These are called auto-adjusting CPAP machines, or APAP. Specifically, APAP is programmed to provide a higher air pressure if it detects resistance in your breathing.
For example, if you change your sleep position during the night, or if you get a congested nose every now and then, then the APAP machine will adapt and provide the optimal air pressure to ease breathing.
Operating a CPAP Machine
To operate a CPAP machine, you wear a mask that fits snugly over your nose and/or mouth. The mask connects to the CPAP machine through a narrow hose. When you turn on the machine, it gently directs filtered, pressurized air into the mask.
Your doctor can help you with how to choose a CPAP mask and also help customize the air pressure. Your doctor usually determines the air pressure based on the results of a sleep study in a clinic. If you find your set pressure level to be uncomfortable, your doctor can reprogram your machine, or you can try a new mask.
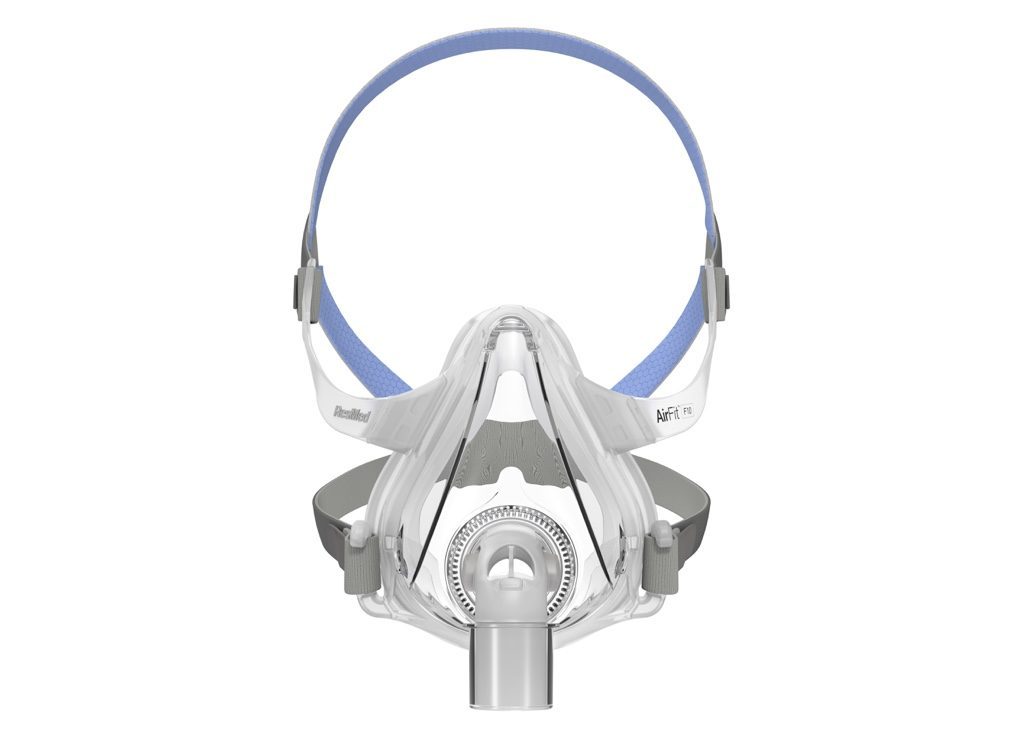
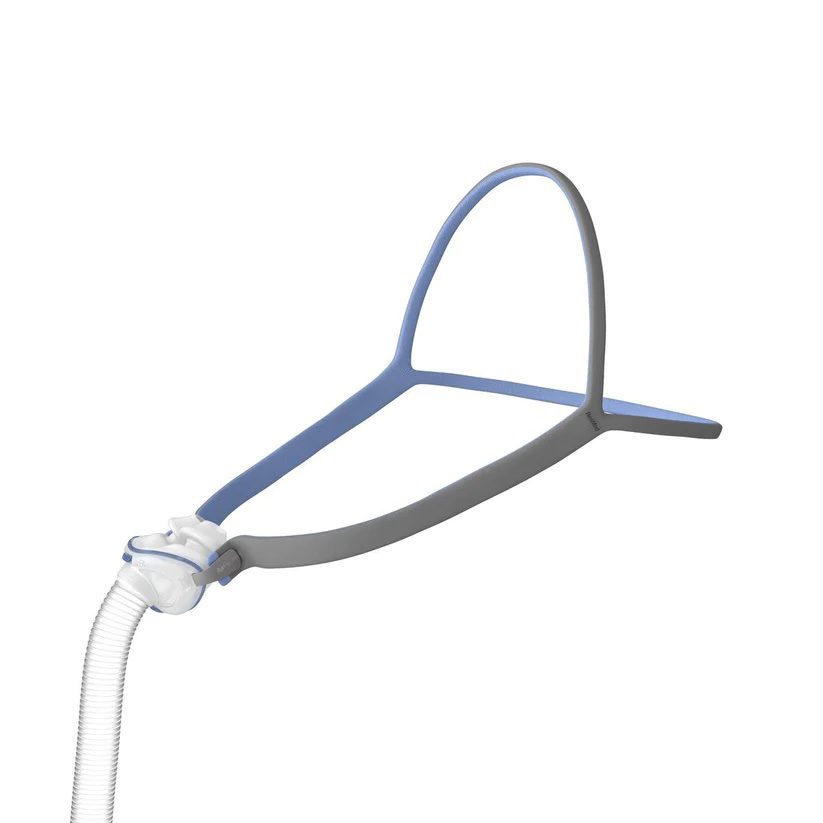
What Are the Different Types of CPAP Masks?
There are a variety of CPAP masks on the market, and you can choose from a wide array of brands.
- Full-face mask: A full-face, also called oronasal, mask covers both the nose and mouth. This mask may suit you best if you breathe mainly through your mouth and if you use a high level of air pressure. Maintaining a good seal to prevent air leakage may be difficult for people with facial hair.
- Nasal mask: A nasal mask covers the nose and extends from the bridge of the nose to the upper lip. It can provide high air pressure levels and can be suitable for people who breathe through their nose at night.
- Nasal pillow: A nasal pillow includes two tubes inserted into the nostrils. Since this mask has little contact with the face, many people find it comfortable. However, it cannot provide higher air pressures like other masks.
Although less common, mouth-only masks are available for people who breathe mainly through their mouths instead of their noses. These masks can be helpful for people who have congested noses or narrow nasal passages.
Benefits of Using a CPAP Machine
Using a CPAP machine may provide several benefits if you have sleep apnea.
- Reduced or eliminated snoring: Snoring is a form of air flow resistance, and it may get better as a result of using CPAP.
- Restorative sleep: Since CPAP prevents mouth and throat tissues from blocking your airway, you are less likely to experience microarousals, or awakenings from deep stages to light stages of sleep. Fewer microarousals means you get more consistent, quality sleep.
- Reduced daytime sleepiness: Because you get more restorative sleep using CPAP, you’ll likely feel less sleepy and more energetic during the day.
- Improved daytime concentration: You may have improved concentration while doing daytime tasks when your sleep improves while using CPAP.
- Reduced blood pressure: CPAP can lower blood pressure and therefore may help slow the progression of serious health problems that are associated with high blood pressure.
- Diabetes prevention: Untreated OSA is associated with insulin resistance and type 2 diabetes. While data on this topic is limited, researchers suspect that CPAP may help regulate insulin and blood sugar levels and possibly prevent and treat type 2 diabetes.
Side Effects of CPAP Machines
While CPAP machines can provide meaningful improvements, they can also have side effects. Fortunately, there are strategies you can take to minimize the effects of CPAP therapy and make treatment more manageable.
- Facial irritation: Sometimes the CPAP mask is not the right fit, and if it’s too tight, it can put pressure on your skin and contribute to sores or ulcers. If this happens, tell your health care provider and start looking for a mask in a different size, a different model, or with a different cushioning material.
- Swallowing air: Swallowing air, also called aerophagia, can result in an upset stomach. Usually, switching to a nasal mask or nasal pillow will relieve this side effect. Alternatively, using an APAP machine or wearing a chin strap to keep your mouth closed while breathing through the nose can help prevent aerophagia.
- Claustrophobia: If you dislike confined spaces, then you may not like the contact a CPAP mask makes with your face. Try a different mask type, such as a nasal pillow, or resize your mask to make sure it fits properly.
- Air leaks: Sometimes if you breathe with your mouth but wear a nasal mask, the air that CPAP pumps into your nose can exit your mouth before it enters your airway. This is called a mouth leak. To resolve this, try wearing a chin strap to keep your mouth closed. You can also consider switching to a full-face mask.
- Nose or mouth dryness: Sometimes CPAP makes your upper airway feel chilly or dry. Adding a humidifier with a heated tube to your CPAP machine may help. If your nose feels stuffy, you could also try a decongestant or steroid nasal spray or switch to a full-face mask.
Other Treatments for Sleep Apnea
Although doctors typically recommend CPAP as a first line treatment, there are other treatment options for sleep apnea. These include alternative types of PAP machines and other therapies.
Your doctor will help you choose the treatment option that works for you, your lifestyle, and preferences. The best choice is the one that improves your symptoms and that you feel comfortable using everyday.
PAP machines
Other types of PAP machines are similar to CPAP in that they deliver pressurized air to keep the airway open, but their different functions make them a better option for some people with sleep apnea.
- BiPAP: A bilevel positive airway pressure (BiPAP or BPAP) machine provides one level of air pressure when you inhale and another level of air pressure when you exhale. In general, BiPAP is typically reserved for people who do not benefit from CPAP or APAP.
- ASV: Adaptive servo-ventilation (ASV) therapy is a treatment for CSA or a mix of CSA and OSA that responds to individual breathing patterns. ASV helps trigger a deep breath if your breathing becomes too shallow or temporarily stops.
- EPAP: A nasal expiratory positive airway pressure (EPAP) device is a simple and lightweight option that may help individuals with OSA. It involves wearing a valve in each nostril as you sleep. When you exhale into the valves, pressure builds up in your upper nasal passages, which helps keep your upper airway open and prepare you for the next inhaled breath.
Oral Appliances
Two oral devices are gaining popularity among people with OSA.
- Mandibular advancement device (MAD): An MAD is a custom-fit, removable device that pushes your lower jaw forward, effectively opening your airway while you sleep. MADs have been shown to be as effective as CPAP at reducing sleep apnea symptoms, but CPAP does a better job of treating breathing disruptions and improving blood oxygen levels.
- Tongue-restraining device (TRD): A TRD is a plastic piece that uses suction to keep your tongue forward and away from your throat. More research is needed on this oral device, but it is an option for people who can’t use an MAD.
There are snoring mouth guards available in stores, but these are not as comfortable or effective as MADs fitted by dentists. The mouth guards sold in stores may provide a false sense of security if they reduce your snoring, but don’t treat your sleep apnea. They may also adversely affect your jaw and the health of your teeth and gums,
Surgery
Surgery may be considered in a few situations for sleep apnea.
Tissues of the nose, mouth, or throat that obstruct the airway in OSA and can be surgically corrected. Other types of surgeries implant a nerve stimulating device to help with breathing.
Although surgery can provide several benefits, such as improvements in snoring, daytime sleepiness, and quality of life, it typically does not completely eliminate OSA. So, after surgery, you may continue to use CPAP or an oral appliance.
When to See a Health Care Provider
Consider contacting your doctor or a sleep specialist if you have signs of sleep apnea, which may include:
- Gasping or choking on air during sleep
- Loud, frequent snoring
- Feeling too sleepy during the day
- Not feeling well-rested after a full night of sleep
- Morning headaches
- Trouble paying attention or remembering things
Since some of these symptoms occur only during sleep, it’s important to take observations by your bed partner seriously.
When you meet with a doctor, they will likely ask you to participate in a sleep study, either in a lab or at home, to determine whether you have sleep apnea. If you are diagnosed with sleep apnea, then your doctor or health care provider may recommend trying CPAP therapy.